Cataract
September 2021
by Ellen Stodola
Editorial Co-Director
The Light Adjustable Lens (LAL, RxSight) offers the unique opportunity to lock in the preferred vision after surgery. With recent updates, the technology can be an attractive option for a variety of refractive cataract patients. Several surgeons discussed how they use this IOL in their practice.
Which patients should the LAL be used for?
As an adjustable toric monofocal IOL, the LAL can be used for any patient who does not want to compromise night vision or contrast sensitivity, and it is particularly well suited for the most challenging refractive patients, said David F. Chang, MD. “These include post-refractive or refractive lens exchange patients, those with unpredictable astigmatism (e.g., mild corneal scars), uncompromising personalities demanding a specific outcome (e.g., no distance [compromise] or no reading glasses), and those who’ve never needed glasses thanks to rigid contact lens monovision and expect this to continue.”
James Loden, MD, said he considers the LAL to be an “upgrade product” in his practice, so the patient pays extra for it. He combines it with one of the femtosecond laser packages in his practice, but he noted that physicians do not need to have a femtosecond laser to be able to use the LAL.
“It’s a way that you can upgrade to a refractive product without having to have the capacity to do corneal relaxing incisions,” he said. “You don’t need a femtosecond laser, and the vast majority of the time, you don’t need an excimer laser to do any fine turning or adjustments of the patient.”
Dr. Loden said it will depend on the practice to see how the LAL fits into the treatment paradigm. He has a large refractive practice and said that this is “absolutely the best technology out there for adjustable monovision.” You can fine tune the patient to exactly what they want with their monovision. “If someone is thinking about monovision and not sure if they’ll tolerate it, you can give them the monovision effect, and if they don’t like it, you can take it away without having to do an invasive surgical procedure.”
He also said that the LAL is a “game changer in operating on prior LASIK eyes and PRK eyes” because you don’t have to overthink the lens implant calculation. You just have to get close with the IOL and let the adjustments do the rest. “It’s dramatically improved patient satisfaction for us in post-LASIK eyes,” he said. “It used to be that on a prior LASIK eye, if the patient wanted a premium product, we had to tell them the chance of having to go back in and do a touch-up was 50–80%, we’re not doing the touch-up until 2 months out, and it would have to be PRK rather than LASIK.”
Deborah Ristvedt, DO, thinks that the LAL came at “a great time where we’re really focusing on precise results and good outcomes for patients.” She uses the lens frequently in post-refractive patients. “It’s nice with this technology where we’re doing all the treatments post-healing,” she said. Additionally, she said it’s a great option for patients with astigmatism. Torics correct astigmatism, but there is still some variability with corneal healing and effective lens position. “I’ve found that to be able to really dial in astigmatism, knowing exactly what axis we’re treating, gave me more confidence that I was going to nail the target every time,” Dr. Ristvedt said. “I’ve found that I’m doing a lot of mini-monovision as well to give patients more extended range of vision.”
Patient discussion
When discussing the LAL as an option with patients, Steven Naids, MD, focuses on a couple of things. First, he explains that while the surgery is the same as with regular cataract surgery, the recovery is quite different.
“I always tell patients that before this, the lens that was put in the eye is what you got, and the recovery was just drops,” he said. “Now, compliance is what matters with the UV glasses. It’s an enormous commitment for the patients to wear the glasses for 6–7 weeks.” You have to get a good feel for the patient and their lifestyle, he said.
Dr. Naids noticed that with more people working from home during the pandemic, they seemed a little more comfortable wearing the glasses at home rather than the workplace.
“We talk about how much work is involved on their end,” he said. “Then we talk about how that is all for long-term gain. In general cases, accuracy is around 60–70%, but now we’re upward of 90%,” he said.
“With every cataract consultation that comes through the doors, we’re always getting biometry and topography,” Dr. Ristvedt said. “We make sure that we’re honing in on technologies where we can start to sort out who are good candidates for different refractive IOL technologies.” She added that she likes to look at the ocular surface and do an osmolarity test, helping identify dry eye, corneal irregularities, higher order aberrations, etc.
“The patient can become confused if we give them too many options,” Dr. Ristvedt said. She likes to keep it simple and ask the patient “How do you want to use your vision?” This helps determine if the patient wants to wear glasses or be less dependent or if the patient prefers to see at distance; distance and intermediate; or distance, intermediate, and near. “I’ve found that with the LAL, I’m using it on patients who want good distance or to correct astigmatism.”
When talking to patients about the LAL, Dr. Chang compares it to putting a golf ball, explaining that IOL power selection requires assumptions and estimates, and he cannot guarantee hitting the target with a single putt. “The LAL gives me three putts, which effectively allows us to also change the target (e.g., the amount of myopia in the second eye) based on the patient’s postoperative experience and function,” he said.

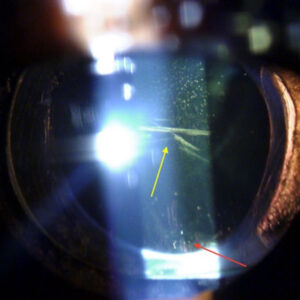
Source: RxSight
Workflow challenges and differences from other IOLs
One major difference that Dr. Chang explained is that he offers every bilateral LAL patient the option of immediate sequential bilateral cataract surgery (ISBCS). “By adjusting both eyes simultaneously postoperatively, they are typically returning the same number of times that immediate sequential patients are for non-adjustable IOLs,” he said.
Dr. Naids noted the importance of having an excellent support staff when doing these cases. You have to have a close team of optometrists and ophthalmologists working together on this, he said, because patients will spend about 2 hours in the office for each treatment.
If you have a post-refractive eye, Dr. Loden said your workload is going to be better than doing a PRK touch-up on top of a LASIK flap. There is less overhead and faster recovery of vision, he said.
But compared to a standard toric lens or standard extended depth of focus lens that you might put in, Dr. Loden said there is an increased workload. “It’s going to take three extra visits to do adjustments and lock-ins,” he added.
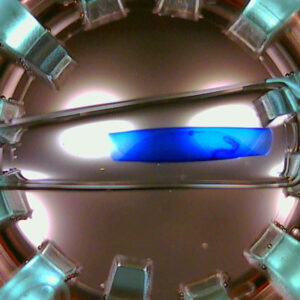
“With the IOL’s ActivShield technology, we’re doing two adjustments and one final lock-in,” he said. Previously, it was two adjustments and two lock-ins, which Dr. Loden said dramatically increased postop time, including traveling to and from the doctor’s office, being dilated each visit, etc. This was a negative part of the experience for the patient, he said, so this update makes the process a little easier.
Dr. Ristvedt noted that with the LAL, there is more chair time post-surgery than pre-surgery. “Postoperatively is where the real work comes in because these patients are coming back more often,” she said, adding that it’s usually after 3–4 weeks that manifest refraction will stabilize. “You want stability before you start to change the lens,” she said, adding that it’s important to make sure the patient understands his or her goals. “Once we start to adjust the lens, they’re coming in every 5–7 days for a recheck,” she said. “It can bog us down a little bit when it comes to doing a precise manifest refraction, checking lifestyle, and dilating enough to make sure we can get a good treatment from the Light Delivery Device (LDD).” Dr. Ristvedt added that there are usually 2–3 treatments before the lock-in occurs.
“I think patients are happy because they have that great vision afterward,” she said. “But it can be a little taxing.”
Diagnostics
Dr. Loden said he doesn’t do anything different in terms of diagnostics for the LAL, noting he obtains Pentacam (Oculus) and IOLMaster (Carl Zeiss Meditec) measurements on every patient. He said it’s also important to know the basic corneal curvature, if the patient has regular or irregular astigmatism, and if they have a healthy retina.
Similarly, Dr. Naids said his preoperative testing is the same for patients who want the LAL. It includes biometry, an OCT of the macula, and corneal topography.
There are some patients—perfectionists and engineers, for example—who agonize preoperatively over what specific refractive target they want, Dr. Chang said. “With the LAL, they can wait to try out their binocular pseudophakic vision postoperatively and confirm or modify their refractive preference based on their daily experience,” he said. “This, and the fact that they won’t have diffractive ring halos, dramatically relieves the anxiety for this type of patient.”
Learning curve and tips
When starting to use the LAL, Dr. Naids said it’s important to be comfortable placing a three-piece lens, and he noted that the injector system is a bit different. He suggested using an eye model to get used to it.
Postoperatively, you have to reassure these patients that their vision is usually not where they want it to be at first and it won’t be for a number of weeks, he said.
Dr. Chang said to think of the LAL as a customizable toric IOL, and the majority of patients will end up with some amount of micro-, mini-, or full monovision. He also suggested that if you don’t want to offer ISBCS, try to do the surgeries close together. The ability to base adjustments on the patient’s binocular, pseudophakic vision is one of the biggest advantages of this technology, Dr. Chang explained.
“This is an easy implementation to pick up,” Dr. Loden said. With the surgery itself, there is basically no learning curve if you’re comfortable implanting a three-piece lens, he said. The only thing that requires a slight learning curve is doing the adjustments.
Recent updates
According to Dr. Loden, a big breakthrough is the ActivShield technology, which is a new UV protective layer built into the LAL. This new UV protective layer is automatically opened by the LDD, allowing precise lens adjustments. When the adjustments are complete, the ActivShield is automatically engaged again to protect the lens from accidental sun exposure. Dr. Loden thinks that in the near term this will increase peace of mind for patients and doctors, and in the long term may be a pathway toward removing the need for UV-blocking glasses.
Dr. Loden added that there has also been a recent upgrade to the software for treatment of astigmatism down to 0.5 D.
Dr. Ristvedt said she thinks ActivShield helps patients and prevents premature lock-in. “I think that’s one of the things that the company has been thinking about,” she said. “They’re thinking about the flow and patients having to be tied to wearing ultraviolet glasses and getting treatments consecutively.”
Dr. Chang also noted the recent FDA approval of the ActivShield. “Although the label still specifies UV glasses, Arturo Chayet, MD, has used this LAL version in a series of patients without them wearing any UV glasses,” Dr. Chang said. “If UV glasses eventually turn out to be unnecessary, this would be a revolutionary advance in the technology.”
He also mentioned that RxSight has developed an EDOF adjustment that could be centered on the visual axis of the near eye postoperatively. “This would be of enormous value in reducing the amount of myopia needed to provide functional reading ability,” he said. “These innovations will make the technology even more attractive to our refractive patients.”
How does Perfect Lens differ from the LAL?
Another adjustable technology in development is Perfect Lens. Dr. Chang said this system would modify the IOL power and design using an in situ femtosecond laser treatment. The technology has been tested in animals and testing in human eyes is just underway, he said.
Dr. Loden said he thinks Perfect Lens and LAL are two very different products. The LAL is a silicone three-piece lens that adjusts its power with UV light. The Perfect Lens is a femtosecond laser that is used to change the refractive index of a lens that has been already implanted in order to adjust the power of the IOL.
Dr. Naids said the idea of the Perfect Lens being able to modify an existing IOL would open up the possibility of lens changes based on patient preference and could help with refractive misses/IOL exchanges. It sounds promising, he said, but he noted that he still thinks LAL will have a place in the treatment paradigm, especially since it’s continuing to get better. “We have something that we know is viable and gives us good results,” he said.
About the physicians
David F. Chang, MD
Clinical Professor of Ophthalmology
University of California, San Francisco
San Francisco, California
James Loden, MD
Loden Vision Centers
Nashville, Tennessee
Steven Naids, MD
Advanced Vision Care
Los Angeles, California
Deborah Ristvedt, DO
Vance Thompson Vision
Alexandria, Minnesota
Relevant disclosures
Chang: RxSight, Perfect Lens
Loden: None
Naids: None
Ristvedt: None
Contact
Chang: dceye@earthlink.net
Loden: lodenmd@lodenvision.com
Naids: steven.naids@gmail.com
Ristvedt: deborah.ristvedt@vancethompsonvision.com