Cornea
December 2020
by Liz Hillman
Editorial Co-Director
The COVID-19 pandemic has affected all areas of medicine, including eye banking. While much more is known about SARS-CoV-2 and the illness it causes, there are still several unknowns that continue to be investigated as they pertain to the safety of donor tissue.
The reduction of corneal surgeries when elective surgeries were canceled and ongoing social distancing decreased the demand for corneal tissue overall, but it has crept back up. Winston Chamberlain, MD, PhD, said in mid-April that tissue demand was down about 90% nationwide; it’s now returned to pre-COVID level in his area. Kevin Corcoran said in June that the U.S. has been fortunate to have a surplus of donor tissue, allowing EBAA eye banks to fulfill requests without delays or waiting lists, but the lack of demand affected every eye bank in the early stages of the pandemic.
Source: EBAA
However, more stringent screening requirements have reduced the overall donor pool by 25–30% and may lead to isolated challenges in providing tissue on demand, Mr. Corcoran continued, adding that the association offers an online platform that allows eye banks with surplus supply to offer it to those that might be in need.
“Stricter donor criteria and enhanced donor screening are in place to ensure donor tissue is safer,” said Clara Chan, MD, explaining that the surgeon has to discuss potential risks with the recipient, similar to how they would with a blood transfusion. “We have done some epidemiological models, which predict a very low likelihood of transmission from donor cornea tissue, approximately <1/109,000 chance. Povidone-iodine is used for 2 minutes twice to clean the ocular surface prior to in situ recovery of corneal tissue.”
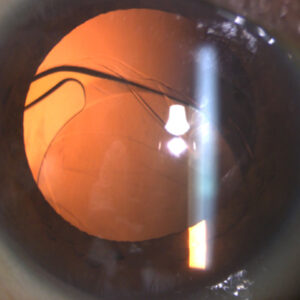
A study of 33 donor corneas that were excluded from surgical use due to not meeting EBAA screening guidelines, medical director review, or a positive COVID-19 test found that of the 20 eyes that came from donors who were positive for COVID-19, three conjunctival swabs, one anterior corneal, five posterior corneal, and three vitreous swabs were positive for the viral RNA.1 The researchers also detected SARS-CoV-2 spike and envelope proteins in corneal epithelium in eyes that were not disinfected with povidone-iodine. The authors of the pre-press study concluded that there is a “small but noteworthy prevalence of SARS-CoV-2 in ocular tissues from COVID-19 donors,” which highlights the importance of donor screening guidelines, post-mortem testing, and povidone-iodine disinfection.
A paper by Desautels et al. on the topic of donor corneal tissue said, “Current recommendations from the United States and global eye bank associations call for the outright avoidance of tissues from donors recently infected with or exposed to COVID-19. This conservative recommendation is currently appropriate given the reported ocular sequelae, tear film viral detectability, and transmissibility of COVID-19.”2
“Several reports have suggested low probability of infectious viral particles in ocular tissue, but real data on risk of transmission from an infected donor are still not known,” Dr. Chamberlain said in a follow-up email to EyeWorld. He pointed to a 2006 study that found ACE2, the host cell receptor that binds SARS-CoV envelope spike protein, in the cornea and conjunctiva. The authors concluded that these cells can bind to the viral spike proteins “slightly.”3
Jennifer DeMatteo noted that, per the FDA, coronaviruses are not known to be transmitted by transplantation of human cells, tissues, or cellular or tissue-based products.
“There have been no reported cases of transmission of SARS-CoV, MERS-CoV, or any other coronavirus via transplantation of ocular tissue,” she said.
As such, she explained that current EBAA standards require double exposure of povidone-iodine to the entire surface of the ocular tissue, resulting in rapid viricidal activity against coronaviruses and reduced likelihood that COVID-19 may be transmitted through corneal transplantation. The EBAA has funded research that will analyze regional infiltration of SARS-CoV-2 in ocular tissues and evaluate the efficacy of povidone-iodine to inactivate the virus within ocular tissue of COVID-19 positive donors, Ms. DeMatteo said. This research will also assess the impact of the pandemic on donor referrals. A second grant from EBAA is funding research that looks at whether the virus can be transmitted through donor corneal tissue.
At this time, to ensure safety of donor tissue, Ms. DeMatteo said eye banks should exclude potential donors who are diagnosed with or suspected to have had COVID-19 or close contact with someone with COVID-19 in the past 28 days. The EBAA released a donor eligibility matrix specifically for COVID-19.
“At this time, the EBAA is not requiring eye banks to perform post-mortem nasopharyngeal RT-PCR testing for SARS-CoV-2. However, a negative PCR result may be necessary (in addition to a medical director review) to release tissue from donors with another etiology to explain their signs and symptoms,” she continued, adding that diagnostic RT-PCR tests for SARS-CoV have not been validated for cadaveric donors and are not intended for donor screening. “The FDA does not currently recommend the use of laboratory tests to screen asymptomatic HCT/P donors.”
Overall, Mr. Corcoran said the pandemic has illustrated that some challenges are better addressed collectively and collaboratively among eye banks, rather than individually.
“[M]any eye banks shared their resources with other banks and with the transplant and healthcare partners in their communities. I think that this spirit will continue to grow within our membership,” he said.
Dr. Chamberlain reiterated in his follow-up email to EyeWorld that while the evidence for SARS-CoV-2 transmission in corneal tissue seems low, there are concerning theoretical risks. “We do need to look carefully in our corneal recipient populations for emergence of COVID after transplantation to see if we can correlate donor risk factors with recipient infection,” Dr. Chamberlain said. “Improved testing with better sensitivity and specificity may give us higher levels of confidence when donors have some risk factors for exposure or signs of respiratory illness. We certainly have to balance our caution to prevent disease transmission with the disposal of safe tissue, which could restore vision in our patients.”
ARTICLE SIDEBAR
Update on COVID-19 and the eye
EyeWorld provided early updates on the research that was coming out of the pandemic regarding the ocular effects, manifestations, and transmission possibilities of SARS-CoV-2. There are now hundreds of peer-reviewed papers published on the topic.
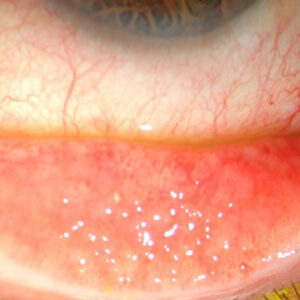
A systematic literature review published in PLoS One identified 16 studies representing more than 2,300 confirmed COVID-19 cases.1 This data showed that 11.6% of these patients had ocular surface manifestations of COVID-19, including ocular pain, discharge, redness, and follicular conjunctivitis. This study also reported viral RNA in 3.5% of ocular samples analyzed. The study authors noted that most published studies on the topic show “significant publication bias and heterogeneity.”
A prospective case series of 32 patients who were positive for COVID-19 evaluated tear and conjunctival samples, collected via swab and analyzed with RT-PCR.2 It found 16% of samples in patients, who did not exhibit conjunctivitis or other ocular symptoms, had viral RNA. Dr. Chamberlain noted a 2003 paper that presented a lower sensitivity of RT-PCR in tear samples, which could mean that rates of ocular infections could be underestimated.3
The role of ocular tissue in transmission of SARS-CoV-2 is likely low, a different systematic literature review concluded, though the eye as an infection route is a possibility.4 One study did show the infection of monkeys with SARS-CoV-2 through an ocular route that later developed into the respiratory disease.5
A study that looked at replication of different viruses in the cornea found that while HSV and Zika do replicate in the cornea, SARS-CoV-2 does not.6 In human corneal explants, SARS-CoV-2 did not replicate at all, according to the authors. “In addition to an antiviral role for IFNλR1 in the cornea, our results suggest that the human cornea does not support SARS-CoV-2 infection despite expression of ACE2, a SARS-CoV-2 receptor, in the human corneal epithelium,” the authors concluded.
References
- Aggarwal K, et al. Ocular surface manifestations of coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis. PLoS One. 2020;15:e0241661.
- Kaya H, et al. Detection of SARS-CoV-2 in the tears and conjunctival secretions of Coronavirus disease 2019 patients. J Infect Dev Ctries. 2020;14:977–981.
- Peiris JSM, et al. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet. 2003;361:1319–1325.
- Peng M, et al. The role of the ocular tissue in SARS-CoV-2 transmission. Clin Ophthalmol. 2020;14:3017–3024.
- Wei D, et al. Ocular conjunctival inoculation of SARS-CoV-2 can cause mild COVID-19 in rhesus macaques. Nat Commun. 2020;11:4400.
- Miner JJ, et al. HSV-1 and Zika virus but not SARS-CoV-2 replicate in the human cornea and are restricted by corneal type III interferon. Cell Rep. 2020;33:108339.
About the sources
Winston Chamberlain, MD, PhD
Petti Associate Professor of Ophthalmology
Casey Eye Institute
Oregon Health & Science University
Portland, Oregon
Clara Chan, MD
Department of Ophthalmology
University of Toronto
Toronto, Canada
Kevin Corcoran
President and CEO
Eye Bank Association of America (EBAA)
Washington, D.C.
Jennifer DeMatteo
Director of Regulations and Standards
Eye Bank Association of America (EBAA)
Washington, D.C.
References
- Sawant OB, et al. Prevalence of SARS-CoV-2 in human post-mortem ocular tissues. Ocul Surf. 2020. Online ahead of print.
- Desautels JD, et al. Risks posed to corneal transplant recipients by COVID-19-affected donors. Ophthalmol Ther. 2020;9:371–379.
- Sun Y, et al. Mechanism of the action between the SARS-CoV S240 protein and the ACE2 receptor in eyes. Int J Ophthalmol. 2006;6:783–786.
Relevant disclosures
Chamberlain: None
Chan: None
Corcoran: None
DeMatteo: None
Contact
Chamberlain: chamberw@ohsu.edu
Chan: clarachanmd@gmail.com
Corcoran: Kevin@restoresight.org
DeMatteo: Jennifer@restoresight.org