For a more recent article on this topic, see “Negative dysphotopsia: How to explain it and management strategies.”
Cover Feature: Pseudophakic dysphotopsia
April 2014
by Vanessa Caceres
EyeWorld Contributing Writer
Treatments linked to suspected causes; prevention remains under investigation
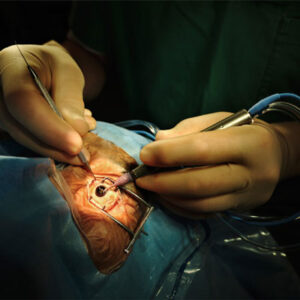
The best way to treat negative dysphotopsia remains a hot topic among surgeons. Negative dysphotopsia that occurs right after cataract surgery is usually best left to resolve on its own. However, if the problem continues a few months after surgery, ophthalmologists must step in to provide a treatment. Their treatment approach usually depends on what they suspect is the cause.
Looking at causes
Negative dysphotopsia appears in patients as a temporal crescent-shaped shadow after in-the-bag IOL implantation following cataract surgery. It was first reported in 2000 by James Davison, MD, cataract and refractive specialist, Wolfe Eye Clinic, with locations throughout Iowa.1 Dr. Davison said he observed the phenomenon with acrylic square-edge IOLs, which were introduced in the 1990s as a way to prevent posterior capsule opacification.
“There’s controversy with the exact mechanism of action,” said David V. Folden, MD, North Suburban Eye Specialists, Minneapolis. “I think more physicians and data would support the fact that it’s ultimately the sharp posterior optic edge design of the modern-day IOL that’s likely the culprit.”
Other suggested factors include an IOL’s high index of refraction, transparency of the peripheral nasal capsule, and type of incision used during surgery.
The immediate postop incidence for negative dysphotopsia appears to be around 20%, said Samuel Masket, MD, in private practice in Los Angeles, and clinical professor of ophthalmology, Jules Stein Eye Institute, David Geffen School of Medicine, University of California, Los Angeles. However, long-term chronic dysphotopsia complaints are closer to 1.5% to 3%, Dr. Masket said.
Surgeons cannot yet predict who will experience negative dysphotopsia, said Jack T. Holladay, MD, clinical professor of ophthalmology, Baylor College of Medicine, Houston.
Dr. Holladay wrote an article in 2011 that used ray tracing diagrams to explain negative dysphotopsia.2
“The peripheral arcuate shadow that patients see is the result of square-edge optics causing a refraction of the rays that pass through the edge of the lens that go in opposite directions (leaving a blind spot), and that creates a shadow. That always happens. If that shadow falls anterior to the functional retina, then you can’t see it. If it falls on the functional retina then you’ll see it,” he said.
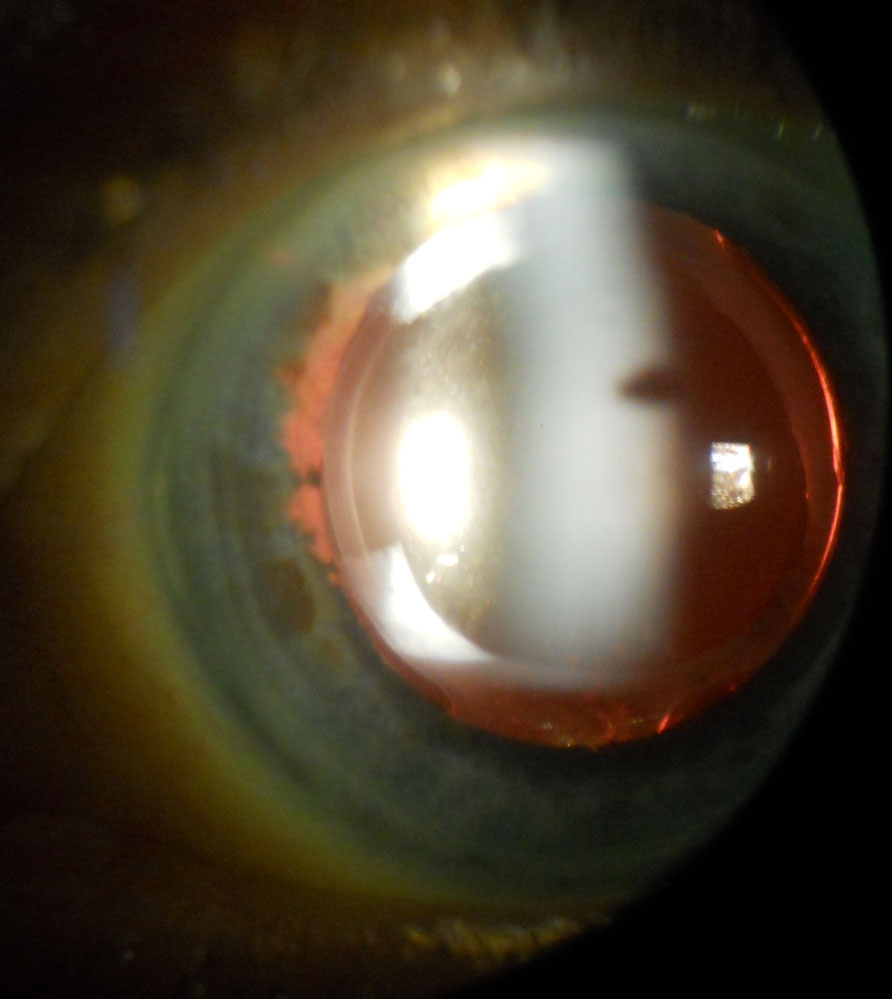
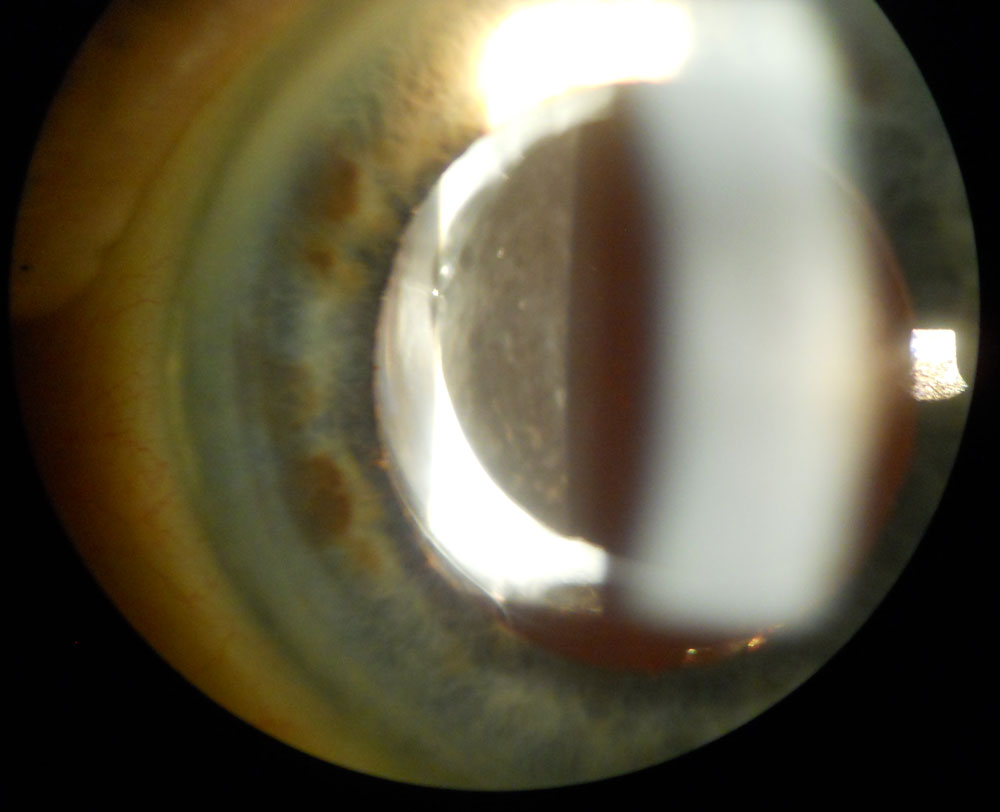
Source (all): David Folden, MD; J Cataract Refract Surg. 2013;39:11101115
“Not everyone’s peripheral retina is at the same point. People who have a functional retina extending far anteriorly will have a higher chance of experiencing this than people who don’t,” Dr. Holladay said. “We have no clinical way of determining how far a patient’s functional retina goes.” However, Dr. Holladay added that if someone experiences negative dysphotopsia in one eye, it’s more likely that he or she will experience it in the fellow eye as well.
Available treatments for negative dysphotopsias
The first recommended treatment for negative dysphotopsia is observation. “Observation is a great first step. Ultimately, we think the capsule peripheral to the optic edge on the nasal side clouds over time, increasing light scatter into that shadow, and that eliminates the negative dysphotopsia,” Dr. Folden said.
If the patient still has the problem 3 to 4 months later, the use of thick-framed glasses or a trial dilation can take place, Dr. Folden said. However, not many patients want to use thicker frames, and dilation is good for diagnosis but not for treatment, he cautioned.
Even if patients must wait a few months before treatment, Dr. Masket reassures them what they are experiencing is a legitimate—and bothersome—visual phenomenon.
A treatment approach published recently by Dr. Folden in one report and David L. Cooke, MD, Great Lakes Eye Care, St. Joseph, Mich., in a separate report is the use of a neodymium (Nd):YAG laser anterior capsulectomy.3,4
Dr. Folden’s study focused on six patients with negative dysphotopsia, five of whom had an Akreos AO M160 posterior chamber (PC) IOL (Bausch + Lomb, Rochester, N.Y.); symptoms completely resolved in three patients and partially resolved in the two others. In one patient who had an AcrySof IOL (Alcon, Fort Worth, Texas), symptoms did not go away.
“Because the anterior capsulectomy did not resolve the symptoms in the patient with the AcrySof IQ toric PC IOL, the anterior capsule should be considered an optical risk factor for negative dysphotopsia and important in the manifestation of symptoms in only some patients,” Dr. Folden wrote. This approach is conservative, Dr. Folden said.
Dr. Cooke’s report focused on negative dysphotopsia that was present in a patient 2 months after receiving a toric plate-haptic IOL that resolved after Nd:YAG removal of a portion of the nasal anterior capsule. The anterior capsule always has a certain degree of translucency and potential for light scatter even immediately following surgery. Light scatter that occurs through the anterior capsule may provide a route for light to reach the sharp posterior optic edge resulting in shadow creation. Although the capsule peripheral to the edge of the optic can help improve symptoms over time, the anterior capsule can contribute to symptoms, and if so, may respond well to Nd:YAG laser anterior capsulectomy.
“In our articles, Dr. Folden and I dramatically improved most cases of negative dysphotopsia with YAG anterior capsulectomy,” Dr. Cooke said. He added that the patient who still had symptoms in Dr. Folden’s report had a toric IOL where the haptics were oriented horizontally instead of vertically. However, Dr. Folden emphasizes that all patients in these two articles received IOLs that had either 360 degrees of sharp posterior optic edge or optic edge discontinuity (at the optic-haptic junction or as in the plate-haptic IOL), all capable of shadow creation regardless of orientation inside the eye. “Unfortunately, some mystery still remains on this topic,” Dr. Cooke said.
Other possible treatments for negative dysphotopsia reported by Dr. Masket and Nicole Fram, MD, Los Angeles, have included the use of a piggyback IOL, a reverse optic capture procedure, and bag for sulcus IOL exchange.5 Drs. Masket and Fram found piggyback IOL implantation and reverse optic capture were the most successful approaches in their study, leading to complete or partial symptom resolution by three months. These results led them to believe that symptoms depend on IOL coverage of the anterior capsule edge. Their study, which included UBM analyses, did not support the concept that increased posterior chamber depth was a causative factor for negative dysphotopsia. Another finding from Dr. Masket: “We’ve found that negative dysphotopsia can occur with any lens so long as it’s in the capsular bag,” he said.
Dr. Masket and H. Burkhard Dick, MD, chairman, University Eye Hospital Bochum, Germany, have tested the Masket Anti-Dysphotopic IOL (Morcher, Stuttgart, Germany) in Europe. The IOL allows for any haptic and edge design as well as toric and multifocal designs. The design features a groove on the anterior optic surface that captures the anterior capsulotomy and allows a portion of the optic to overlap the capsulorhexis. Dr. Masket has recently received a U.S. patent for the IOL design, which also received a CE mark last year. It’s been used investigationally in five patients, none of whom have experienced negative dysphotopsia, Dr. Masket said. He believes that the IOL design, which mimics an aspect of reverse optic capture, will help patients avoid negative dysphotopsia.
Another IOL called the bag- in-the-lens IOL from Marie-Jos Tassignon, MD, Antwerp, Belgium, similarly prevents negative dysphotopsias. However, use of that lens involves the performance of a posterior capsulotomy, which many surgeons would prefer to avoid so as to not risk encountering vitreous, Dr. Holladay said.
The IOLs from Dr. Masket and Dr. Tassignon are under use or experimentation outside the U.S.
Lens exchange is yet another possible treatment. When Dr. Davison encounters negative dysphotopsia, he will remove the lens, put in a silicone rounded IOL, and perform an optic capture. He said he has tried using the Nd:YAG laser but it did not help, although he acknowledges that others have found success with it.
Although negative dysphotopsia does not occur often, Dr. Davison said surgeons still wish that they could find ways to prevent the problem.
References
- Davison JA. Positive and negative dysphotopsias in patients with acrylic intraocular lenses. J Cataract Refract Surg. 2000;26:1346-1355.
- Holladay JT, Zhao H, Reisin CR. Negative dysphotopsias: The enigmatic penumbra. J Cataract Refract Surg. 2012;38:1251-1265.
- Folden DV. Neodymium:YAG laser anterior capsulectomy: Surgical option in the management of negative dysphotopsia. J Cataract Refract Surg. 2013;39:1110-1115.
- Cooke DL, Kasko S, Platt LO. Resolution of negative dysphotopsia after laser anterior capsulotomy. J Cataract Refract Surg. 2013; 39:1107-1109.
- Masket S, Fram N. Pseudophakic negative dysphotopsia: Surgical management and new theory of etiology. J Cataract Refract Surg. 2011;37:1199-1207.
Editors’ note
Dr. Holladay has financial interests with the Holladay IOL Consultant, Abbott Medical Optics (Santa Ana, Calif.), and WaveTec Vision (Aliso Viejo, Calif.). Dr. Masket designed the Masket Anti-Dysphotopic IOL mentioned in the article. He has financial interests with Alcon (Fort Worth, Texas). The other physicians interviewed have no financial interests related to their comments.
Contact
Cooke: davidlcooke@gmail.com
Davison: jdavison@wolfeclinic.com
Folden: foldav@gmail.com
Holladay: docholladay@docholladay.com
Masket: avcmasket@aol.com