Cornea: Best practices
July 2023
by Liz Hillman
Editorial Co-Director
It’s not uncommon for cornea specialists to come across a glaucoma patient in need of an endothelial transplant, and the management of these patients from preop through long-term postop has certain nuances. EyeWorld spoke with Sophie Deng, MD, PhD, and Nir Sorkin, MD, for their insights on how to best manage glaucoma patients who need lamellar keratoplasty.

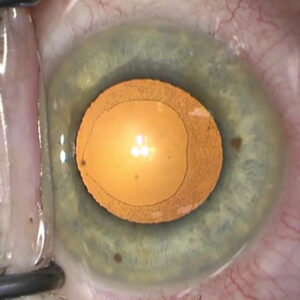
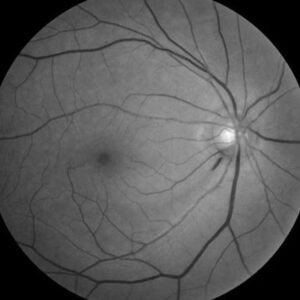
Source: Sophie Deng, MD, PhD
Glaucoma and endothelial cell loss
A number of studies have looked at glaucoma and associated endothelial cell loss. One suggests that there are several hypotheses for why this can occur, including direct compression of the endothelium due to high IOP and medication toxicity.1 Dr. Sorkin shared that another reason for decompensation could be due to the prior surgeries these patients might have received to treat their glaucoma (such as cataract surgery, trabeculectomy, or tube shunts).
“Multiple procedures may affect their cornea, and that’s when we come into the picture,” Dr. Sorkin said of cornea specialists.
When it comes to DMEK or DSAEK, Dr. Sorkin and coauthors published a paper that found the 4-year graft survival rate was similarly low between the two, but DMEK resulted in better visual acuity.2 For this reason, Dr. Sorkin said he performs DMEK unless otherwise contraindicated for the patient.
A study published in 2017 found that eyes with previous trabeculectomy or tubes had good short-term outcomes, with a 0.9% rejection rate over a follow-up of 9.7±7.3 months.3 Dr. Deng said her success rate in the short term is similar for patients with glaucoma as it is to those without. Long-term graft survival is a different story. In a series of 251 consecutive DMEK procedures performed by Dr. Deng, secondary graft failure at a mean 38.4±11.2 months was 41.5%, 0%, and 2.4% in eyes that had prior glaucoma surgery, eyes with medically treated glaucoma, and eyes without glaucoma, respectively.4 Endothelial cell loss was higher in prior surgery eyes as well, 63.8%, compared to 47.6% for eyes medically treated for glaucoma and 44.0% for eyes without glaucoma.

Source: Sophie Deng, MD, PhD
Preop considerations
When assessing a glaucoma patient for lamellar keratoplasty (of which Dr. Sorkin said DMEK is his preference provided there are no other comorbidities that should preclude it), both Dr. Sorkin and Dr. Deng said that ensuring the patient’s IOP is well controlled is the first step.
“Often these patients have IOP well above their target IOP, and I send them back to their glaucoma specialist,” Dr. Deng said.
Compliance on glaucoma medications is also important, Dr. Sorkin said.
“After [DMEK] surgery, we put them in a state where their glaucoma control may be jeopardized because we’re giving them long-term steroid therapy that can affect the pressure. You have to have them well controlled. … We don’t want to put another factor into the equation if they’re not stable,” Dr. Sorkin said.
Dr. Deng said that the patient should be able to add at least two IOP-lowering medications to their regimen prior to DMEK surgery because they might need them to manage an increased IOP postop due to corticosteroid use.
In addition to medication considerations, Dr. Sorkin said that if the glaucoma patient has a tube, the position of that tube in the anterior chamber should be considered because it could interfere with the graft. If it’s too long, it should be trimmed prior to or in combination with DMEK surgery. The tube could also be repositioned to put it posteriorly, Dr. Sorkin said. He said there is speculation that when the tube is too close to the graft, aqueous flow could damage the endothelium, reducing the length of graft survival. Other factors also negatively affect the long-term survival of corneal transplants in eyes with prior trabeculectomy and shunt, Dr. Deng said.
Surgical considerations
When it comes to DMEK surgery in patients with glaucoma, Dr. Deng said that eyes with prior tube shunts or trabeculectomy might have anterior or posterior synechiae that needs to be lysed during the DMEK procedure.
Dr. Sorkin said both of these filtration procedures could also filter out the air that is needed for the graft attachment more quickly. He said a bigger air fill might be needed or the patient can be positioned afterward in such a way to reduce this chance.
Dr. Deng said that she doesn’t change much of what she does preop, intraop, or postop for patients who have had prior MIGS vs. trab/tube.
Postop considerations
Both Dr. Deng and Dr. Sorkin emphasized the importance of regular IOP monitoring in the postop period for DMEK patients who have glaucoma. Dr. Deng said she will check IOP 1–2 hours after DMEK surgery in the postop area, and she has a low threshold to burp the paracentesis to lower the IOP if it is over the mid-20s at the bedside using a portable slit lamp.
Dr. Sorkin also cautioned against a high IOP in the early postop period, due to the air bubble potentially blocking the trab and/or causing pupillary block.
“If I see a big air fill, especially a couple of hours after surgery when I check these patients, I will have a lower threshold for removing some of the air at the slit lamp to avoid reaching the status of pupillary block because I don’t want them to have an IOP spike,” he said.
He also said that when measuring IOP in the early postop period, try to use a low to no-contact tonometer to avoid potentially dislocating the graft.
Later in the postop period, IOP needs continued monitoring due to the prolonged steroid use. Dr. Deng and Dr. Sorkin said that the cornea specialist and glaucoma specialist, which in some cases might be the same surgeon, should collaborate and communicate on whether a steroid drop needs to be reduced or postponed or if additional glaucoma management should be added.
“If the IOP is not controlled by medication, additional glaucoma surgery might be necessary,” Dr. Deng said.
Finally, Dr. Sorkin said that glaucoma patients need to be counseled about some different things. First, he said it should be very clear that they need to continue their glaucoma regimen even after the addition of steroid drops; he said patients can sometimes become confused and discontinue one for the other. Second, he said there is a need to understand the high long-term failure rate of grafts when patients have a trab or tube.
“They need to know there is a high chance the graft will fail every few years, and they’ll need to get repeat grafts. You need to have that conversation with the patient so that they know what to expect,” Dr. Sorkin said.
About the physicians
Sophie Deng, MD, PhD
Joan and Jerome Snyder Chair in Cornea Diseases
Cornea Division
Stein Eye Institute
University of California, Los Angeles
Los Angeles, California
Nir Sorkin, MD
Director of Cornea and Anterior Segment Research
Department of Ophthalmology
Tel Aviv Medical Center and Tel Aviv University
Tel Aviv, Israel
References
- Gagnon MM, et al. Corneal endothelial cell density in glaucoma. Cornea. 1997;16:314–318.
- Alshaker S, et al. Four-year survival comparison of endothelial keratoplasty techniques in patients with previous glaucoma surgery. Cornea. 2021;40:1282–1289.
- Aravena C, et al. Outcomes of Descemet membrane endothelial keratoplasty in patients with previous glaucoma surgery. Cornea. 2017;36:284–289.
- Bonnet C, et al. Long-term outcomes of Descemet membrane endothelial keratoplasty in eyes with prior glaucoma surgery. Am J Ophthalmol. 2020;218:288–295.
Relevant disclosures
Deng: None
Sorkin: Beyeonics
Contact
Deng: deng@jsei.ucla.edu
Sorkin: nir.sorkin@gmail.com