Glaucoma: Back to basics
September 2022
by Ellen Stodola
Editorial Co-Director
Ensuring that the ocular surface is optimized is a key step before cataract surgery, but it is also important in the context of glaucoma. Inder Paul Singh, MD, and Peter Wu, MD, discussed the importance of addressing the ocular surface and what to do prior to glaucoma surgery and combined cataract/glaucoma procedures.
Dr. Singh said he is passionate about making sure his colleagues understand the impact of the ocular surface on patient quality of life, compliance, and overall control of glaucoma. In general, there are few other conditions in the eye that have as many associated symptoms as ocular surface disease, i.e., tearing, fluctuating vision, light sensitivity, pain, and foreign body sensation.
“When we tell patients, ‘Here’s a drop’ and don’t address or acknowledge dry eye, patients often blame the glaucoma drops for their ocular surface symptoms, which in turn leads to less compliance, more side effects, and the potential for fluctuating pressure.”
Inder Paul Singh, MD
When dry eye patients are symptomatic and we treat glaucoma with topical drops, we end up adding more preservatives and chemicals to the surface, potentially exacerbating symptoms, Dr. Singh said. “When we tell patients, ‘Here’s a drop’ and don’t address or acknowledge dry eye, patients often blame the glaucoma drops for their ocular surface symptoms, which in turn leads to less compliance, more side effects, and the potential for fluctuating pressure,” he said.
Dr. Singh spoke about a non-published study that found when the ocular surface is addressed, symptoms explained to patients, and dry eye treated, patients are able to be on fewer medications and achieve target IOP. “We saw 50% of patients on less medications,” Dr. Singh said, partially due to compliance.
Dr. Singh said he took 20 patients sent to him for uncontrolled glaucoma who had signs or symptoms of ocular surface disease. He used a questionnaire to determine OSDI score and symptomology. These were patients with mild to moderate glaucoma who had significant ocular surface symptoms.
Dr. Singh then took the patients off glaucoma drops and had them return in 6 weeks. The pressures didn’t increase as much as he thought they would when off the medications (an average of a 15% increase). The patients’ dry eye was treated with cyclosporine, MGD therapy, and other treatments. At follow-up, symptoms significantly improved. Patients then restarted their prostaglandin analog once a day. After a year of follow-up, Dr. Singh said almost 48% were at target on one drop, while the average patient was on 2.3 medications. This decreased the drop burden by 50%. “We think part of that is because of compliance, patient satisfaction, and improved quality of life by getting rid of drops and treating dry eye,” he said.


Source: Inder Paul Singh, MD
The patients also exhibit increased confidence in their physician when ocular surface symptoms are explained to them. “One of the biggest mistakes that a lot of our colleagues make, especially in the glaucoma world, is that they think they’re not a dry eye center and don’t have time to treat dry eye,” Dr. Singh said. Physicians don’t have to spend hours looking at diagnostic tests for dry eye to be able to help these patients. It’s about symptomology, he said, adding, “Many times when we diagnose patients, it isn’t staining or other diagnostic signs, it is often symptomology, such as fluctuating vision or tearing.” Asking simple questions, like if the patient’s vision comes and goes when blinking or after reading and if they have blurry vision when watching TV or looking at the computer, has helped Dr. Singh identify and address the surface issues.
Since his study, Dr. Singh said he has become aggressive in looking for these issues, and compliance is a big issue. He thinks the number one comorbidity that affects compliance is dry eye.
Additionally, he mentioned that ocular surface disease causes significant surface inflammation. Immunosuppressants and steroids help calm this inflammation down. There are also studies that show some patients with allergic conjunctivitis have trabeculitis, inflammation not just on the surface of eye but also the trabecula. “My theory is there are some people with significant dry eye where pressures aren’t controlled,” he said. “You treat dry eye and put them back on drops and their pressures are better controlled.” This could be attributed to the inflammatory cascade. “I think there might be an impact on the outflow itself with inflammation from ocular surface disease, and if we can treat that, we may theoretically have a better chance of helping outflow,” he said.
If there is inflammation on the surface of the eye, and the surgeon is planning to do a trabeculectomy or subconjunctival surgery, there is a greater likelihood of bleb failure. This is why it’s important to address the ocular surface, whether by the of use SLT, drug delivery, or early MIGS to reduce medication burden.
Dr. Singh added that prostaglandin analogs have been shown to affect the meibomian glands and cause gland dropout. It’s not just the preservatives, it’s the chemical in the glaucoma drops that can also cause significant destruction to the glands in the lids and conjunctiva.
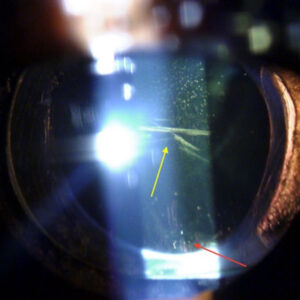
In addition to symptomology, there are certain tests that can identify dry eye in the office. For example, he said that one simple addition is to use a Wratten filter on the slit lamp. This helps accentuate and highlight the ocular surface and tear film, he said. “Even if you use fluorescein, it’s hard to see staining when you put a drop in because it’s a high volume of drop. But if you use the Wratten filter, it will highlight the tear film more aggressively, and you can see staining and tear film breakup time better than just using cobalt blue light,” Dr. Singh said.
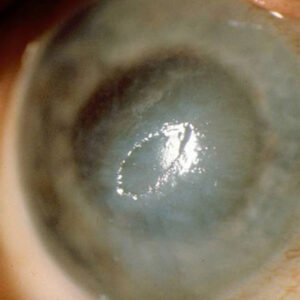
Dr. Wu, a cornea specialist, noted that he often sees limbal stem cell deficiency in his glaucoma patients, particularly those on multiple glaucoma medications. This can be caused by toxicity from the benzalkonium chloride (BAK) preservatives used in the glaucoma medications but can be seen in other ocular conditions and chronic contact lens wearers as well.
Dr. Wu encourages his glaucoma patients to lubricate the ocular surface with preservative- free artificial tears as much as possible. “This is often hard for my glaucoma patients, as they are already on multiple drops for their glaucoma,” he said. “For my glaucoma patients with signs of limbal stem cell deficiency or ocular surface issues, I try to make sure they are on preservative-free formulations of their glaucoma medications. If the limbal stem cell deficiency is more advanced or if there are significant ocular surface issues, I often incorporate other treatments, such as autologous serum eye drops or amniotic membranes to optimize the ocular surface as much as possible.”
The majority of MIGS procedures are done at the same time as cataract surgery, Dr. Singh said, and many of these patients are paying extra money for premium lens options; they expect and deserve good outcomes. If the ocular surface is not healthy, outcomes may not be optimal and recovery may take longer.
Dr. Wu said he talks to his glaucoma patients with significant ocular surface disease and stresses that the surface of the eye needs to be optimized before proceeding with cataract surgery. “This is important to get the best result possible with their cataract surgery,” he said. “This can sometimes take months, especially with patients with advanced ocular surface disease.”
[template id=14580]Prior to doing cataract surgery on his glaucoma patients, Dr. Wu makes sure the topography is regular with minimal to no signs of ocular surface disease on exam. “I like to make sure that my intraocular lens biometry correlates with my topography as well,” he said. “If there is an issue with the ocular surface, I will repeat the biometry after treating the ocular surface until I see consistency in the readings, especially if I’m planning to implant a toric lens.”
The time for ocular surface optimization preop depends on how bad it is, but Dr. Singh estimates about a month. He will usually put patients on lifitegrast or cyclosporine, and some type of MGD treatment option. He also will use steroids like loteprednol to calm the surface. “If they need an urgent subconjunctival surgery like trabeculectomy or the XEN Gel Stent [Allergan], you might not want to wait that long,” he said; even 1–2 weeks could be enough time to calm the inflammatory cascade.
Dr. Singh said Durysta (bimatoprost intracameral implant, Allergan) can help get patients off drops a few months before surgery to improve the surface. Even for patients not having surgery, Dr. Singh has used Durysta for a drug holiday. It releases bimatoprost for a period of 4 months, but the duration can be longer—6 months to 2 years with one implant. Overall, Dr. Singh said he’s had positive patient experiences with this approach. Though it doesn’t last forever, it does get patients off their medications for a few months and gives the surface time to heal. “I think Durysta is a great alternative and a stopgap solution for those patients who are having dry eye issues,” Dr. Singh said.
Dr. Singh said there are many treatments like intense pulsed light (IPL) therapy, TearCare (Sight Sciences), LipiFlow (Johnson & Johnson Vision), BlephEx, and more that can be useful for MGD treatment, Dr. Singh said.
Dr. Singh stressed that even glaucoma-focused surgeons can help patients with ocular surface problems by identifying the problem and educating patients about why they have symptoms. That’s half of the battle, he said; don’t minimize the impact dry eye can have on patients’ quality of life and ability to stay compliant.
About the physicians
Inder Paul Singh, MD
The Eye Centers of Racine & Kenosha
Racine & Kenosha, Wisconsin
Peter Wu, MD
Sacramento Eye Consultants
Sacramento, California
Relevant disclosures
Singh: Allergan, Alcon, Bausch + Lomb, Glaukos, New World Medical, Nova Eye, Novartis, Sight Sciences
Wu: None
Contact
Singh: ipsingh@amazingeye.com
Wu: pwu@saceye.com