Cornea: Back to basics
September 2022
by Liz Hillman
Editorial Co-Director
Aqueous tear deficient dry eye and evaporative dry eye—distinguishing between the two, knowing when both are at play, and treatment options are of growing importance as more patients are identified with some form of dry eye and as certain refractive procedures depend on a healthy ocular surface.
Source: Cynthia Matossian, MD
“Dry eye is ubiquitous. It is common to see patients with dry eye disease of all different severities,” said Cynthia Matossian, MD. “It is no longer the post-menopausal woman who has this diagnosis. The face of dry eye is changing, and it is becoming more common in younger ages, including patients in their 20s and 30s. It increases in prevalence and incidence with age, [and] there are a number of contributing factors.”
Dr. Matossian, Preeya K. Gupta, MD, and Vatinee Bunya, MD, MSCE, shared their insights on the nuances of diagnosis and treatments for evaporative and aqueous tear deficient dry eye.
Evaporative dry eye
Evaporative dry eye, Dr. Matossian said, stems from some form of meibomian gland dysfunction. Identification starts with being a good listener, she said. Questionnaires can be filled out by patients ahead of their visit or in the office, and technicians can be helpful contributors to this process as well.
“Technicians can be empowered to ask questions, and we need to become astute listeners because our patients truly don’t know how to express what’s going on. Often they say their vision is blurry and think they need new spectacles when the reason for the blurry vision is the dry eye,” Dr. Matossian said.
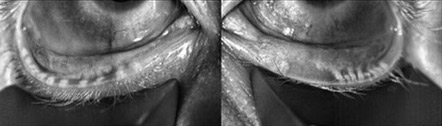
When warranted, point-of-care testing should be done, Dr. Matossian continued, noting that this could include meibography, MMP-9 testing, ocular surface and tear osmolarity testing, and a slit lamp exam with vital dyes. She also said to look, lift, push, pull (LLPP), per the ASCRS Cornea Clinical Committee’s Preoperative OSD Algorithm. “Looking at the quality and expressibility of the meibum helps identify these patients,” Dr. Matossian said.
In terms of treatment, Dr. Matossian said the first step is patient education.
“If the patient does not understand what’s going on, they’re not going to be compliant with anything we recommend to them, let alone pay cash for their deductibles of prescription medications or cash-pay in-office procedures,” she said.
Dr. Matossian thinks oral omega-3 supplementation is important for improving the quality of the meibum. From there, keep the orifices of the meibomian glands open with procedures like microblepharoexfoliation and at-home remedies with lid scrubs including tea tree oil or hypochlorous acid.
“These all work in combination and synergy together,” she said, adding that use of a heated moisture mask not only keeps the gland orifices open and but also helps with the viscosity of the meibum.
From there, Dr. Matossian discussed in-office treatments that heat and can help evacuate the glands, such as the TearScience LipiFlow (Johnson & Johnson Vision), Systane iLux2 (Alcon), and TearCare (Sight Sciences).
What a physician brings into practice for treatment of evaporative dry eye depends on their level of comfort and how comprehensive a dry eye center the physician/practice has, Dr. Matossian said.
“Having many of these devices is beneficial because dry eye is so variable. For example, some patients who are claustrophobic might not do well with the LipiFlow, and they might do better with an open eye procedure, such as the Systane iLux2 or TearCare,” she said. “Other patients who would prefer an automated system with a technician standing away and not having a manual expression component might prefer the LipiFlow.
“Having multiple options is the best, but every practice does not have to go all out and buy every option available,” she continued. “My recommendation would be to start small. Start with one procedural treatment, one diagnostic treatment, and build as your dry eye practice expands.”
Dr. Matossian noted that even with daily at-home treatments and the intermittent in-office procedures, dry eye patients can experience flares. She said most evaporative dry eye patients have flares several times a year, triggered by external environmental stressors, like allergies, airplane travel, increased screen time, etc. She said there is now an FDA-approved product, Eysuvis (loteprednol, Kala Pharmaceuticals), for these cases.
Aqueous tear deficient dry eye
When asked about diagnosing aqueous tear deficient dry eye, Dr. Gupta noted that most patients have mixed-mechanism dry eye disease—some component of aqueous tear deficient and some component of evaporative.
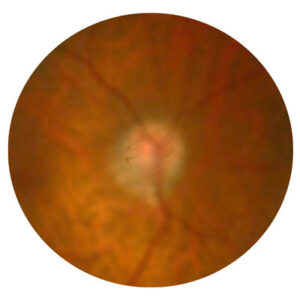
“At its outset, I think it’s less critical that we complicate the issue with is it aqueous/is it evaporative, and we should just assume that patients often suffer from some component of both,” she said. “That said, for aqueous deficient … the eye is not producing the aqueous layer of the tear film robustly. The aqueous is produced by the lacrimal gland. The more modern way of thinking of the tear film, rather than the more traditional three layers of the tear, is thinking of it as two layers: the lipid layer and the muco- aqueous layer.”
With reduced aqueous production, the overall tear volume decreases, Dr. Gupta said. “You can imagine how if you don’t have the volume of tears, it’s hard for it to spread across the surface, and it’s hard for it to appropriately lubricate the ocular surface.”
Aqueous deficiency can be identified by looking at tear volume or tear meniscus height. Dr. Gupta said ophthalmologists should also have their “antennas up” for patients who could be at risk for aqueous deficiency: those with autoimmune diseases like Sjogren’s or other diseases where the lacrimal gland could be attacked and reduce its aqueous secretion. If a patient doesn’t have a diagnosed autoimmune disease, Dr. Gupta said it’s important to keep in the back of your mind if you’re identifying aqueous deficiency. She said it’s important to ask patients about other body symptoms because Sjogren’s, for example, is “not common, but it’s not uncommon.”
“[We need to do] our due diligence to help patients get a diagnosis if it is present because it can change their systemic outlook as well, not just their dry eyes,” Dr. Gupta said.
Dr. Bunya said ocular surface staining and Schirmer’s testing can be used, the latter with or without anesthesia.
“For any patient who is being evaluated for possible Sjogren’s disease, it is important to perform the Schirmer’s test without anesthesia, as this is the test that is included in the classification criteria for Sjogren’s disease,” she said. “Also, it’s important to remember that aqueous tear deficient dry eye patients often also have evaporative dry eye, and therefore, it’s important to look for signs of blepharitis and meibomian gland dysfunction in all dry eye patients. For example, Sjogren’s patients, who classically are thought to have aqueous tear deficient dry eye, often have the best clinical outcomes when both causes of dry eye are treated.”
The first-line treatment for aqueous deficiency is to increase lubrication with artificial tears, gels, or ointments, Dr. Bunya said, adding that for those with moderate to severe disease, she recommends preservative-free varieties. If patients are still symptomatic after additional lubrication, she mentioned several prescription drops that are available: topical cyclosporine (Restasis [Allergan] or Cequa [Sun Pharmaceutical]) and topical lifitegrast (Xiidra [Novartis]).
Dr. Bunya continued that no prescription eye drop has been proven to be superior over the others, so it’s often a matter of trial and error to find what works for specific patients. She noted that insurance coverage can be a hurdle.
Both Dr. Bunya and Dr. Gupta discussed Tyrvaya (varenicline, Oyster Point), a nasal spray that stimulates the trigeminal nerve pathway for tear production. Dr. Gupta described how Tyrvaya not only stimulates the lacrimal gland but also causes contraction of the meibomian gland muscle and degranulation of the goblet cells, which produce mucin.
[template id=14580]“It’s stimulating the complete tear. We like to think of this product as something that’s trying to restore tear film homeostasis. When that happens, you’re basically independent of the etiology, whether it’s evaporative or aqueous deficient,” she said.
Dr. Bunya and Dr. Gupta also mentioned punctal occlusion or cautery. Dr. Gupta noted that plugs in the right person can be helpful, but they won’t aid patients with evaporative dry eye or allergies.
Other available treatments for aqueous tear deficient dry eye, Dr. Bunya said, include short courses of topical steroid drops; blood products, such as autologous serum eye drops; and scleral lenses.
‘There is no cure’
In the end, all the physicians interviewed for this article said the treatments for dry eye will need to be lifelong to maintain symptom relief.
“There is no cure, and I’m very open with my patients. They need to understand that,” Dr. Matossian said. “It is a chronic condition for which they will need treatment forever. Their symptoms will improve if they stay compliant with their daily regimen.”
Dr. Bunya said that while patients will likely be on some sort of treatment for life, once they find an effective regimen, it can greatly improve their quality of life.
“In addition, dry eye has received increased interest from pharmaceutical companies in recent years, so I am hopeful that with more research, we will find more effective therapeutic options,” she said.
About the physicians
Vatinee Bunya, MD, MSCE
William F. Norris and George E. de Schweinitz Associate Professor of Ophthalmology
University of Pennsylvania
Philadelphia, Pennsylvania
Preeya K. Gupta, MD
Managing Director
Triangle Eye Consultants
Cary, North Carolina
Cynthia Matossian, MD
Founder
Matossian Eye Associates
Doylestown, Pennsylvania
Relevant disclosures
Bunya: None
Gupta: Allergan, Novartis, Oyster Point
Matossian: Alcon, BlephEx, Johnson & Johnson Vision, Physician Recommended Nutriceuticals, Sight Sciences
Contact
Bunya: Vatinee.Bunya@pennmedicine.upenn.edu
Gupta: preeyakgupta@gmail.com
Matossian: CMatossianMD@icloud.com