ASCRS News
September 2022

Pain control and reduction of opioid use associated with intracameral phenylephrine/ketorolac 1.0%/0.3% administered during cataract surgery
Eric Donnenfeld, MD, Daniel Mychajlyszn, Andrey Mychajlyszyn, Rebecca Stein, MD
This study sought to compare pain and the need for pain management with an opioid during cataract surgery when phenylephrine/ketorolac 1.0%/0.3% (P/K) or epinephrine (control) was used intraoperatively. Patients were randomized to receive intracameral P/K or epinephrine in their first eye and the opposite in their second eye 2 weeks later for the bilateral surgery. The primary endpoint of the study was the need for fentanyl during surgery for pain. Fifty-six patients were enrolled. The authors reported that significantly fewer eyes in the P/K group (12.5%) required intraoperative fentanyl for pain compared to the epinephrine group (33.9%). Pain scores were lower in the PK group compared to the epinephrine at all time points during the study. According to the study, 85.7% of patients who received P/K had “no pain to mild pain” during surgery compared to 58.9% who received epinephrine. Slightly more than 82% of patients who received P/K did not receive intraoperative fentanyl and reported experiencing “no pain to mild pain” compared to 58.9% in the control group. The authors concluded that use of P/K reduced pain and the need for intraoperative opioids.
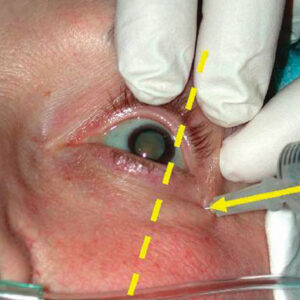
Bilateral simultaneous postoperative endophthalmitis (BSPOE): Review of cases reported over the past 50 years
Mike Yuan Chen, BMSc, Susan Ruyu Qi, MD, Steve Arshinoff, MD, FRCSC
All previously published reports of bilateral simultaneous postop endophthalmitis since 1970 were retrospectively reviewed, with seven cases being reported after immediately sequential bilateral cataract surgery (ISBCS). The authors reported that in most of these cases, the surgical protocol recommended by the International Society of Bilateral Cataract Surgeons was “breached or uncertain.” The authors concluded that cases of bilateral postop endophthalmitis were rare and their causes varied. “Strict adherence to the iSBCS General Principles of Excellence in ISBCS, 2009 surgical protocol and care with operating room construction seem to considerably lessen the risk,” the authors stated.
Defocus curves: Focusing on factors influencing assessment
Thomas Kohnen, MD, PhD, FEBO, Jessie Lemp-Hull, DrPH, Raj Suryakumar, BS (Optom), PhD, FAAO
Investigators sought to evaluate the factors that influence assessment of defocus curves and the different methods used to analyze defocus curves. The authors reported that there is a lack of standardization that can limit cross-study comparisons of defocus curves. Factors influencing defocus curves, according to the authors, include pupil size, contrast level, sphere vs. cylinder defocus, viewing distance, monocular vs. binocular assessment, Snellen vs. logMAR charts, and diopter range and step. The authors stated that while “defocus curves are a proven and effective method for determining a patient’s range of vision and are of particular use for differentiating the performance of presbyopia-correcting IOLs,” it is “important to understand the impact of these factors and ensure testing is standardized, especially in study designs that assess the performance of different IOL technologies.”
A randomized, prospective clinical study evaluating dexamethasone intraocular suspension 9% vs. prednisolone acetate 1% in controlling postoperative pain and inflammation in patients undergoing bilateral sequential cataract surgery
John Hovanesian, MD, Eric Donnenfeld, MD
Thirty patients (29 included in analysis) were enrolled in a contralateral eye study that compared patient preferences and pain when they received intracameral moxifloxacin/dexamethasone suspension followed by topical bromfenac for 30 days (1-drop regimen) to their second eye experience, which received topical moxifloxacin 0.5% QID for 7 days, bromfenac 0.07% daily for 30 days, and prednisolone acetate 1% QID for 30 days (3-drop regimen). The authors found that 96.6% of patients preferred the 1-drop regimen, self-reporting less pain on this regimen as well as less interference in their activities and out of pocket costs. Inflammation and postop day 1 UCVA were also better, according to the investigators, with the 1-drop regimen. The macular thickness and IOP were similar between the two groups.
Ophthalmologists’ attitudes toward immediate sequential bilateral cataract surgery (ISBCS): a Dutch national survey
Lindsay Spekreijse, MD, Claudette Veldhuizen, MD, Ype Henry, MD, Frank van den Biggelaar, PhD, Carmen Dirksen, PhD, Rudy Nuijts, MD
The attitudes and practice patterns of members of a Dutch ophthalmic society regarding immediately sequential bilateral cataract surgery (ISBCS) were evaluated via a national survey. A total of 520 surveys were sent and 237 responded overall (227 of whom provided data on ISBCS). At the time, 62 (27.3%) performed ISBCS but most in a low-volume capacity (about 1–5 patients per month). Nearly 50% (108 ophthalmologists, 47.6%) reported considering ISBCS more routinely in the future. The availability of separate products and instruments for both eyes as well as the advantage to the patient were important, according to the respondents, when considering ISBCS. Reasons for not currently performing ISBCS were mainly endophthalmitis risk and potential for legal risks.
Geographic variations in gender differences in cataract surgery volume among a national cohort of ophthalmologists
Cindy Cai, MD, Janek Klawe, MA, Sumayya Ahmad, MD, Scott Zeger, PhD, Jiangxia Wang, MS, Grace Sun, MD, Pradeep Ramulu, MD, PhD, Divya Srikumaran, MD
A retrospective study of a 2012–2018 Medicare database revealed gender disparities in cataract volume. These disparities in volume among male and female surgeons have not changed over time, the authors found. According to the data, there were 8,480 cataract surgeons, 78% of whom were male. These male surgeons were more likely to work in areas that were considered more “deprived,” which the authors noted could explain, in part, some of the volume disparity by gender. The authors found that cataract surgeries per office was greater for males than females in all years in the South, Midwest, and West, but not in the Northeast. The authors suggested further studies to better understand and address gender disparities in cataract surgery volume among surgeons.