Glaucoma
July 2021
by Liz Hillman
Editorial Co-Director
Glaucoma, while vision threatening, should not necessarily be an immediate contraindication to premium cataract surgery technologies, such as toric and presbyopia-correcting IOLs and FLACS. Reay Brown, MD, Paul Harasymowycz, MD, and Joey Hsia, MD, said there are situations where these technologies are suited for glaucoma patients, but the decision to offer them is not as straightforward.
“New IOL technology always comes last to glaucoma patients,” Dr. Brown said. “Part of this makes sense—these are difficult eyes with small pupils, denser cataracts, shallow chambers, etc. But some of the adoption delay is unfounded fear. Most glaucoma patients have fairly routine cataracts and would benefit greatly from toric lenses, femto, and sometimes multifocal lenses.”

Source: Paul Harasymowycz, MD
Toric IOLs
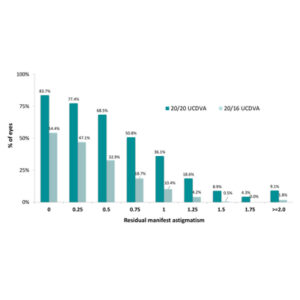
The physicians said it’s well established that toric IOLs provide the opportunity for good uncorrected visual acuity without a reduction in contrast sensitivity. In 2015, Brown et al. published a retrospective case series of 126 eyes of 87 patients who had glaucoma and corneal astigmatism.1 Patients received an AcrySof Toric IOL (Alcon). The investigators found a mean UDVA of 0.04±0.08 logMAR, 98% achieved 20/40 UDVA or better, and 47% 20/20 or better. Refractive cylinder was reduced from a mean of 1.47±1.10 D preop to 0.31±0.37 D postop, with 97% of eyes having residual refractive cylinder of 1 D or less, 90% of eyes 0.75 D or less, and 83% of eyes 0.5 D or less.
Dr. Brown said any glaucoma patient with central acuity could benefit from a toric lens. “In our study of toric lenses in glaucoma patients, there was a substantial group of patients who had extensive visual field loss including split fixation. They did very well with toric IOLs,” Dr. Brown said, adding that he recently completed a study of patients who had split fixation with advanced visual field loss. “Toric lenses enabled even that group to achieve excellent uncorrected central acuity.”
Dr. Brown offered his favorite example of toric success. He said the patient had only a partial central island of vision remaining and nearly 4 D of astigmatism. He used a T9 toric IOL (Alcon), which helped the patient reach 20/20 uncorrected acuity.
Dr. Harasymowycz said angle surgery, such as trabecular stents or tissue removal surgery, does not significantly alter axial length or corneal curvature. Thus, “our glaucoma patients can most definitely benefit from correction of their astigmatism,” he said.
Traditional filtering procedures can change astigmatic measurements, so Dr. Harasymowycz said it’s worth delaying cataract surgery until axial length and astigmatism are stable. He said with glaucoma patients on topical drops it’s important to treat ocular surface disease for reliable topographic and biometric measurements to ensure patient satisfaction.
“Often surgeons forget to verify the standard deviation of their biometry or the Placido disc images of their topographers. Macular pathology is also not infrequent in the glaucoma population, and a normal macular OCT is important before considering toric IOLs,” Dr. Harasymowycz said.
Dr. Hsia said if a trabeculectomy is in the patient’s future and they need cataract surgery first, he wouldn’t use a toric due to the potential for refractive instability. Those with pseudoexfoliation glaucoma with preop or intraop signs of zonulopathy are poor candidates for torics due to the potential for IOL complex dislocation.
Dr. Harasymowycz thinks glaucoma patients can be overlooked and not offered premium technology due to their potentially blinding disease. When it comes to torics, the opposite should be true. He said with reduced contrast sensitivity and visual fields, glaucoma patients often “greatly appreciate any improvement in their vision.”
Presbyopia-correcting IOLs
While torics might be a safe bet for many glaucoma patients, presbyopia-correcting IOLs require more nuanced discussion. Dr. Hsia offers newer generation presbyopia-correcting IOLs to glaucoma patients who are motivated to reduce spectacle dependence. He described newer presbyopia-correcting IOLs as pupil size independent with improved contrast sensitivity profiles that are on par with monofocal IOLs.
“With appropriate consultation and patient selection, presbyopia-correcting IOLs can be safely offered to glaucoma patients and achieve excellent visual outcomes as well as an improvement in their quality of life,” he said, noting that factors that impact his decision are age, type/stage/stability of glaucoma, refractive stability, and ocular surface disease.
Older patients with stable, controlled, pre-perimetric or mild POAG, or chronic angle closure glaucoma with a healthy ocular surface are candidates for presbyopia-correcting IOLs in Dr. Hsia’s practice. He said he’ll often recommend an angle-based MIGS in conjunction to reduce glaucoma medications.
Patients with moderate glaucoma and peripheral field defects are more controversial candidates for these lenses, but Dr. Hsia thinks with proper counseling and IOL selection, they can succeed. Dr. Hsia avoids presbyopia-correcting IOLs in advanced or uncontrolled glaucoma patients, those with signs of zonulopathy, and in younger patients due to uncertainty of future glaucoma control.
Dr. Harasymowycz said some of his happiest outcomes are glaucoma patients who have received a presbyopia-correcting IOL. Glaucoma stage is most important in considering their candidacy, with OCT to assess ganglion cell loss, in addition to their visual field status.
“The best contrast for distance visual acuity is with monofocal IOLs, followed by EDOF IOLs, and bi- or trifocal IOLs decrease the amount of available light for distance visual acuity,” Dr. Harasymowycz said. “I will only offer the latter in patients with no visual field damage and very little ganglion cell loss, in whom it is unlikely that their glaucoma will progress, and usually only in one of their eyes. We tell our patients that because of their glaucoma, we want to give them the best quality of distance vision possible. Our myopic patients are often disappointed to lose their near visual acuity, and in mild glaucoma we offer an EDOF IOL while warning them that they are likely to need reading glasses.”
Both Dr. Harasymowycz and Dr. Hsia said surgeons often hesitate to offer presbyopia-correcting IOLs to glaucoma patients.
“Though newer generation IOLs provide good bench data compared with monofocal IOLs, there is still a paucity of research with glaucoma patients,” Dr. Hsia said. “As more research data sheds light on this topic, we will likely see a paradigm shift in the use of presbyopic IOLs with glaucoma patients.
“As a side note, I think surgeons should be comfortable with IOL exchange when placing presbyopia-correcting IOLs,” Dr. Hsia continued. “Despite careful counseling and selection, there will be patients who are unhappy with the results and may require IOL exchange.”
FLACS
Dr. Harasymowycz said he regularly performs FLACS on glaucoma patients. He noted that most lasers used for this purpose do not raise IOP as high as that for LASIK. The weaker zonules present in many glaucoma patients make the prefragmentation of the nucleus with the laser an attractive feature. Bubbles generated in FLACS can also pneumodissect the lens and thus reduce hydrodissection. Dr. Harasymowycz has used FLACS on patients who’ve had glaucoma filtering procedures but said care must be taken to avoid suction rings on thin and ischemic blebs. Use a small suction ring size to avoid pressure peripheral to the limbus, he said.
Dr. Hsia generally avoids FLACS in glaucoma patients because several studies have found no benefit of FLACS over traditional phaco. Pupillary dilation challenges can preclude FLACS in these patients, and he noted concern of transient IOP elevation from FLACS potentially damaging ganglion cells in advanced patients. He said FLACS could be useful in cases with weak zonules and/or a shallow anterior chamber, such as pseudoexfoliation glaucoma, angle closure glaucoma, and traumatic glaucoma.
When it comes to offering premium cataract surgery technology to glaucoma patients, Dr. Brown said, “they deserve the very best we have to offer to help them achieve the best possible uncorrected vision.”
Dr. Harasymowycz said there are advancements coming in the field that could even help patients regain some lost vision. “As technology is evolving at a rapid pace and we may be reversing ganglion cell and optic nerve damage, it is important to treat them as if they may eventually regain some of their vision,” he said.
About the physicians
Reay Brown, MD
Atlanta Ophthalmology Associates
Atlanta, Georgia
Paul Harasymowycz, MD
Associate Professor
University of Montreal
Quebec, Canada
Joey Hsia, MD
Assistant Professor of Ophthalmology
University of California, San Francisco
San Francisco, California
Reference
- Brown RH, et al. Toric intraocular lens outcomes in patients with glaucoma. J Refract Surg. 2015;31:366–372.
Relevant disclosures
Brown: None
Harasymowycz: Alcon, Bausch Health, Johnson & Johnson Vision
Hsia: None
Contact
Brown: reaymary@comcast.net
Harasymowycz: pavloh@igmtl.com
Hsia: Joey.Hsia@ucsf.edu