Cover Feature: Secondary glaucoma challenges
May 2015
by Vanessa Caceres
EyeWorld Contributing Writer
Subset of disease is not always easy to diagnose or treat
Although pigmentary glaucoma is not as common as other forms of primary open angle glaucoma, specialists still tend to see it regularly and must choose the best treatment.
“It’s one of those things that the more you look for it, the more you find it. The trick is it can be very subtle, especially earlier on,” said Robert J. Noecker, MD, clinical assistant professor, Yale University, and in private practice, Ophthalmic Consultants of Connecticut, Fairfield, Conn.

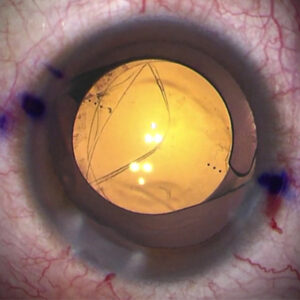
Source: Robert J. Noecker, MD
Pigmentary glaucoma classically appears in younger, myopic males. It can develop as young as the late teens or early 20s, said Robert Ritch, MD, Shelley and Steven Einhorn Distinguished Chair, professor of ophthalmology, New York Eye and Ear Infirmary, New York. Dr. Ritch pioneered much of the early research into pigmentary glaucoma, and he has previously reported that it is seen in 2.45% of the Caucasian population.
The condition is often hereditary, which is why Paul Harasymowycz, MD, chief of glaucoma, University of Montreal, and director, Montreal Glaucoma Institute, recommends that those with pigmentary glaucoma have their siblings or children examined, especially if they are myopic.
Dr. Harasymowycz finds that younger, active patients are more likely to experience a “pigment storm,” leading to a sudden increase in the number of pigment granules that can be associated with an IOP spike and a secondary blurring of vision. “In these patients, we sometimes ask them to run up and down a flight of stairs at the office and see if we can exhibit this phenomenon, especially if present on history,” he said.
It is important for glaucoma specialists to distinguish between primary and secondary pigment dispersion, Dr. Harasymowycz said. “In secondary pigment dispersion, the lens must be dealt with if one wants to avoid progressive pigment shedding,” he said.
A careful differential diagnosis is also crucial, said Brian A. Francis, MD, professor of ophthalmology, Doheny Eye Institute, University of California, Los Angeles. Other conditions that might appear similar include pseudoexfoliation syndrome, uveitic glaucoma, and ocular tumors, he said. “If someone has an iris melanoma, that releases pigment that can mimic pigmentary glaucoma, especially if it is unilateral,” he said.
Pigmentary glaucoma and cataract surgery
The need to perform cataract surgery in patients with pigmentary glaucoma may not be common, as they tend to be younger. However, medical therapy may accelerate the development of cataract, Dr. Harasymowycz said.
“In some ways, with modern cataract surgery, you can argue that you’d have a lower threshold for doing cataract surgery because one, you can fix the refractive error, and two, you can change the way the iris is contacting the lens and the structures behind it,” Dr. Noecker said.
He sees value in performing a laser iridotomy and cataract surgery to stop a large amount of pigmentary dispersion. “If the patient is still in a phase where pigmentary dispersion is causing damage, it’s good to alter the course of that,” he said.
Patients with pigmentary dispersion syndrome may be helped by the irrigation and aspiration during cataract surgery, with the subsequent “washing out” of the trabecular meshwork pigment, Dr. Harasymowycz said.
Dr. Ritch cautions against clear lens extraction in these patients as they tend to be young.
If cataract surgery is necessary, Dr. Francis shares the pearl of avoiding reverse pupillary block during surgery by putting an instrument under the iris at the pupil and tenting it up as irrigation is turned on. This will help make the anterior chamber stable.
Surgeons should also inform these patients that they are at a higher risk for retinal detachment post-cataract surgery. When Dr. Harasymowycz observes that the posterior vitreous face is still attached to the retina via optical coherence tomography or when peripheral retinal changes are noted during a preop exam, he will often send the patient to a retina colleague, who can evaluate the necessity of pretreating certain areas with a laser.
“This also serves as an important step in potential future medico/legal situations that may arise if complications do occur,” he said.
Treating pigmentary glaucoma
The treatment for pigmentary glaucoma tends to vary according to the patient and the surgeon—there is no one go-to procedure, Dr. Francis said.
Brian A. Francis, MD
“The treatment for pigmentary glaucoma tends to vary according to the patient and the surgeon—there is no one go-to procedure. In general, it’s somewhat more difficult to control than open angle glaucoma, but we still use the same types of medications and surgeries.”
“In general, it’s somewhat more difficult to control than open angle glaucoma, but we still use the same types of medications and surgeries,” he said. Although laser trabeculoplasty is an option, surgeons have to be mindful of pressure spikes because there is a lot of pigment in the angle, and the laser energy is taken up more easily. “You have to use a lower power and consider doing a lesser number of shots. Instead of doing 360 degrees, you may do 180 degrees,” Dr. Francis said. Then, watch the patient and see if the procedure needs to be repeated at a later time.
In the latter situation, Dr. Harasymowycz advises remeasuring the IOP 30 to 45 minutes after laser, seeing patients back sooner if the IOP is elevated, and giving oral carbon anhydrase inhibitors if tolerated. “It may not be advisable to offer selective laser trabeculoplasty (SLT) to patients with heavily pigmented trabecular meshwork, especially if they have uncontrolled IOPs and are already on multiple IOP-lowering drops,” he said.
Trabeculectomy and tube shunts are also an option. “With trabeculectomy, you have to be careful because of the risk for hypotony. That’s where MIGS has a role,” Dr. Francis said. “MIGS procedures where you remove or bypass the trabecular meshwork will be fairly effective.”
“You have to decide if MIGS will be adequate in getting the pressure down,” Dr. Noecker said. “Anything working with outflow is helpful. There’s a move to do more MIGS versus just doing a trabeculectomy. It’s reasonable to start with SLT or a MIGS procedure that’s safe to do, but it may not lower the IOP enough. Other procedures that eliminate the trabecular meshwork may have the best indication.”
Some MIGS procedures may have to be used off-label if there is not a coexistent cataract, Dr. Francis said. Another consideration is whether a patient wants to continue using contact lenses, which are common in these mostly myopic patients, Dr. Harasymowycz said.
“Clearly, MIGS procedures such as trabeculectomy with the Trabectome [NeoMedix, Tustin, Calif.], 360-degree trabeculotomy with sutures, or the iTrack catheter [iScience, Menlo Park, Calif.], or trabecular bypass procedures with the iStent [Glaukos, Laguna Hills, Calif.] may be less invasive and safer options,” Dr. Harasymowycz said, noting that the latter surgeries have been found to be more effective when combined with cataract extraction.
Pigmentary glaucoma tends to get better with age, remission usually beginning in the mid-40s with the onset of presbyopia, Dr. Ritch said. So, while patients with other types of glaucoma may see worsening of their symptoms in their 50s or by age 60, those with pigmentary glaucoma tend to find their condition has improved.
Editors’ note
Dr. Francis has financial interests with Allergan (Irvine, Calif.), AqueSys (Aliso Viejo, Calif.), Endo Optiks/Beaver Visitec (Waltham, Mass.), Lumenis (Yokneam, Israel), and NeoMedix. Dr. Harasymowycz has financial interests with Alcon (Fort Worth, Texas), Abbott Medical Optics (Abbott Park, Ill.), Bausch + Lomb (Bridgewater, N.J.), and Ivantis (Irvine, Calif.). Dr. Noecker has financial interests with Glaukos and Endo Optiks. Dr. Ritch has financial interests with Aeon Astron (Leiden, the Netherlands), Sensimed (Lausanne, Switzerland), iSonic Medical (Paris), Allergan, and Ocular Instruments (Bellevue, Wash.).
Contact information
Francis: BFrancis@doheny.org
Harasymowycz: pavloh@igmtl.com
Noecker: noeckerrj@gmail.com
Ritch: ritchmd@earthlink.net