Cataract
July 2015
by Lauren Lipuma
EyeWorld Staff Writer
Retinal surgeons are exploring novel ways to prevent post-vitrectomy cataracts
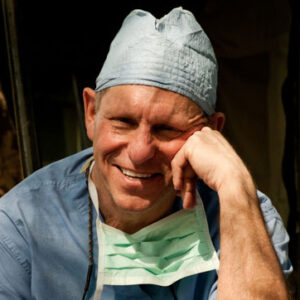
“Now that we know it’s oxygen, we have to develop some mechanism for preventing oxygen from reaching the lens.”
Nancy Holekamp, MD
Cataract formation is such a common complication of vitrectomy that in many cases, it makes sense to combine macular surgery with phacoemulsification rather than performing the surgeries sequentially.
“If you do a vitrectomy, 95% of people are going to get accelerated post-vitrectomy nuclear sclerotic cataracts and require cataract surgery within 2 years,” said Nancy Holekamp, MD, associate professor of clinical ophthalmology and visual sciences, Washington University School of Medicine, St. Louis.
Many physicians agree that combining the 2 procedures provides better outcomes and decreased risk for the patient, but Dr. Holekamp believes that there is an even better option—modifying vitrectomy surgery to prevent cataract formation in the first place. Over the past several years, retinal surgeons have uncovered the mechanism behind post-vitrectomy cataract formation, and Dr. Holekamp believes they can now use that knowledge to develop novel surgical techniques to protect the lens from opacification.
The oxygen hypothesis
“The only way to prevent cataract formation is to understand what causes cataract formation,” Dr. Holekamp said. “And what causes cataracts is oxygen.”
Oxygen coming from the highly vascularized retina enters the posterior segment and encounters the vitreous. The vitreous absorbs that oxygen and protects the anterior ocular structures—including the lens—from oxidation.
“The price you pay for taking a breath every day of your life is that a little bit of that oxygen works its way to the crystalline clear lens and causes it to oxidize,” Dr. Holekamp said. “It rusts, like iron rusts or a cut up apple turns brown sitting on the kitchen counter.”
The vitreous consumes oxygen and protects the lens from oxidation—so long as it’s a gel, Dr. Holekamp said. As the vitreous slowly liquefies with age, more oxygen circulates in the posterior chamber, causing a slowly progressive nuclear sclerotic cataract to form. When the vitreous is surgically removed, oxygen reaches the lens more quickly, resulting in a rapid acceleration of nuclear sclerotic cataract formation.
The idea that oxidation causes cataract formation has come to be known as the oxygen hypothesis, an idea that has emerged only within the last several years. Now that retinal surgeons understand this process, Dr. Holekamp said, they can begin to develop strategies to prevent it.
“Now that we know it’s oxygen, we have to develop some mechanism for preventing oxygen from reaching the lens,” she said.
Potential solutions
The vitreous consumes oxygen because it has high levels of ascorbate, Dr. Holekamp said, so implanting a drug delivery device that delivers ascorbate to the vitreous cavity could restore its ability to consume oxygen and protect the lens.
Ophthalmologists at the University of Louisville are exploring another option—placing a clear barrier behind the lens at the time of surgery. Working with bioengineers, they have designed a biocompatible hydrogel that can be injected behind the lens during vitrectomy. So far, the bioengineered gel has served as a successful oxygen barrier in animal models, but it has not yet been tested in human eyes. The researchers hope to test the gel in clinical trials within the next year, according to a press release from the University of Louisville.
The ultimate solution would be to provide a vitreous substitute with gel-like properties, Dr. Holekamp said, or to inject small molecules into the vitreous that would reform the natural gel.
Researchers at Purdue University are currently studying the protective effect of biomimetic proteoglycans in cartilage degradation, a method that could be adapted to treat the vitreous, Dr. Holekamp said. Although they differ in function, cartilage and vitreous share many structural similarities—they are extremely hypocellular tissues that begin as firm, gel-like substances that slowly liquefy over time.
“These strategies at this point are hypothetical, but they’re rational strategies because we now understand what causes post-vitrectomy cataracts,” Dr. Holekamp said. “And once we understand what causes post-vitrectomy cataracts, we can actually understand what causes age-related cataracts. So we should be able to devise strategies or methods for preventing age-related cataracts—that’s the end game.”
Conducting more research on the vitreous will be key to developing these techniques, Dr. Holekamp said. “No one is doing research on this area,” she said. “If more people knew about this, maybe we could get more young people interested in studying the vitreous gel or exploring these possibilities. I think this is the next frontier in ophthalmology research.”
Editor’s note
Dr. Holekamp has no financial interests related to this article.
Contact informartion
Holekamp: nholekamp@gmail.com