Cataract/IOL
March 2011
by Maxine Lipner
Senior EyeWorld Contributing Editor
Keying in on conditions that can cause double vision
Pre-existing strabismus and a family history of this are two red flags to look for when trying to head off diplopia in cataract patients, according to Kammi B. Gunton, M.D., assistant surgeon, Wills Eye Institute, Philadelphia. Investigators led by Dr. Gunton reported on the incidence and causes of diplopia following cataract and refractive surgery in the September 2010 issue of Current Opinions in Ophthalmology.
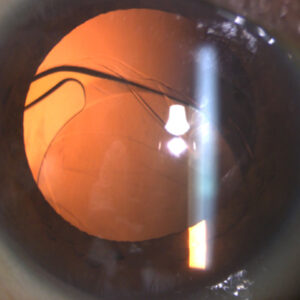
Source: Gary L. Fanning, M.D.
Retrospective review
Diplopia is a rare problem, but Wills Eye Institute hosts an adult strabismus clinic, and double vision tends to occur more frequently in patients here. “At this point there are eight different physicians at Wills who see adult patients with double vision,” Dr. Gunton said. “We wanted to see what the underlying causes are for people who have double vision.”
Since there were not enough patients from Wills Eye alone, investigators opted to conduct a literature search on this. “We didn’t have enough data to do a study of just our patients,” Dr. Gunton said. “We decided to do a literature search to see if we could help the people in our service and give them an idea of what the causes and treatments are.” The hope was to help practitioners zero in on what works and what doesn’t.
In addition, investigators wanted to alert general practitioners about potential red flags that could lead to diplopia following surgery. “There are certainly patients who are more likely to have double vision after cataract surgery,” Dr. Gunton said. “I wanted to make sure that practitioners are aware of the red flags.”
This retrospective study keyed in on cataract surgeons who had recorded double vision in their patients, as well as strabismus specialists with patients who had double vision.
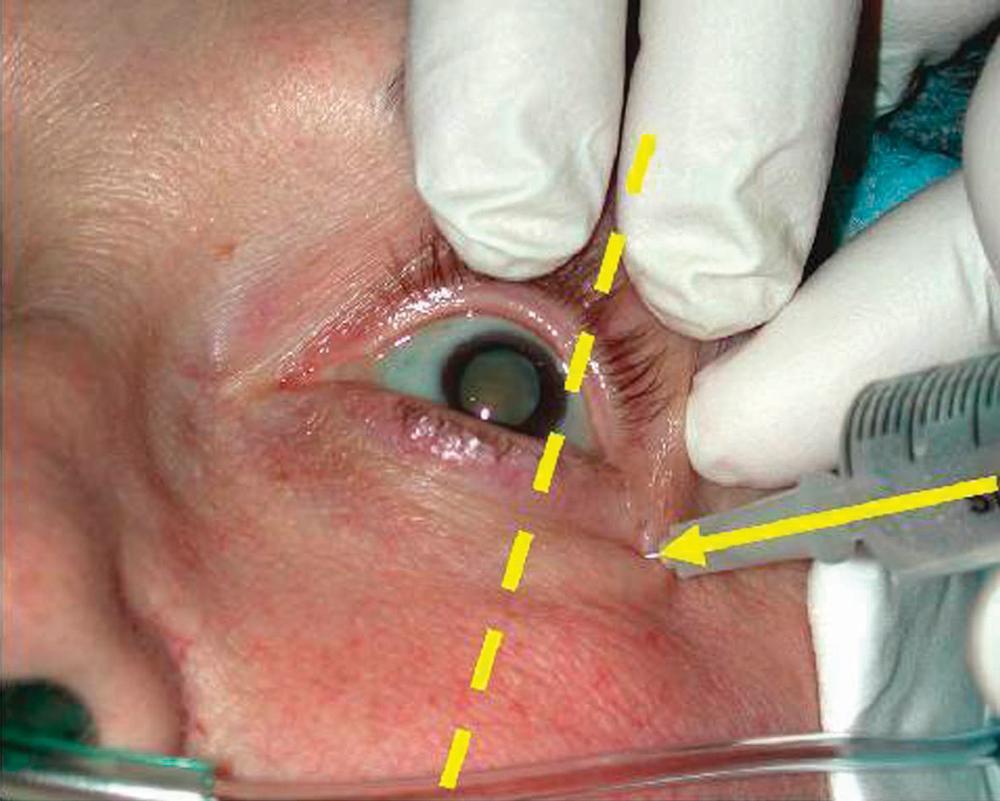
Investigators reported that following retrobulbar anesthesia for cataract extraction, the incidence of diplopia ranged from 0.23-0.98%. However, in case series involving topical anesthesia, there was an incidence ranging from 0-0.21%.
Red flags
Strabismus ultimately turned out to be a major red flag. “The most common cause of double vision following cataract surgery was pre-existing strabismus that had been controlled and then decompensated following cataract surgery,” Dr. Gunton said. “If there is any history of strabismus, practitioners should warn these patients that they may have double vision afterward.”
In addition, Dr. Gunton thinks that it’s important to ask if other family members are strabismus sufferers. Approximately one-quarter of the patients in the study were found to have a family history of strabismus as well. “They may have something that is underlying that you don’t know about,” Dr. Gunton said.
The patients’ glasses in some cases may tell a story. “Another way to predict diplopia is shockingly simplelook and see if patients have any type of prism in their glasses,” Dr. Gunton said. “Sometimes it’s quite small and patients forget about it.”
Investigators also found that systemic diseases, such as a thyroid condition, can be the culprit. “Even if they don’t have thyroid eye disease, those patients could end up having some type of strabismus problem,” Dr. Gunton said. “Again, it was probably something that was small and underlying that decompensated when we manipulated their vision system.”
When it came to treatment, there was good news. “It is treatable,” Dr. Gunton said. “For most of these patients you can do strabismus surgery and the double vision goes away.”
The study also delved into double vision following refractive surgery with LASIK. Dr. Gunton found that this occurred far less frequently and appeared to have a different origin. It usually occurs in just one eye and is linked to a corneal aberration that can occasionally occur following refractive surgery, Dr. Gunton explained.
She hopes that practitioners come away from the study with a better understanding of current causes of surgically related diplopia. “Prior to topical anesthesia, the most common cause of double vision used to be injection into a muscle with a local anesthetic, and that is becoming very rare,” Dr. Gunton said. “Some practitioners may think that since we’re not using injection anesthesia, no one gets double vision any more and we don’t have to worry about it.” This study, however, discounts that. “We’re showing that even in cases of topical anesthesia, there are still patients who have double vision, and there are some red flags to watch for,” Dr. Gunton said.
Overall, when it comes to refractive surgery, Dr. Gunton stressed that questions remain. “This is something that is going to come up more frequently as more people have refractive surgery, and I think that we don’t understand it well enough,” she said. “I think that we probably have to look at this a lot more.”
ARTICLE SIDEBAR
Study: Brimonidine-timolol fixed combo reduces IOP after phaco
A fixed brimonidine-timolol combination has been shown to reduce IOP in patients 6, 12, and 24 hours after phacoemulsification surgery, according to a study published in the February issue of the Journal of Cataract & Refractive Surgery. The study, led by Nikolaos Pharmakakis, M.D., was a prospective, randomized, comparative case series conducted at Greece’s Patras University Hospital department of ophthalmology. Patients scheduled for phaco were randomized into two groups. The treatment group (28 eyes) received one drop of brimonidine-timolol combination immediately after surgery, while the control group (30 eyes) received no treatment.
According to the published results, the mean IOP increased by 0.14 mm Hg±3.88 (SD) (P=.88) in the treatment group and increased by 2.8±5.01 mm Hg (P=.007) in the control group. Twelve hours after surgery, the mean IOP decreased by -0.57±3.82 mm Hg (P=.49) in the treatment group and increased by 2.20±4.56 mm Hg (P=.009) in the control group. Twenty-four hours after surgery, the mean IOP decreased by -1.57±2.30 mm Hg (P=.012) in the treatment group and increased by 0.86±4.21 mm Hg (P=.175) in the control group.
Editors’ note
Dr. Gunton has no financial interests related to her comments.
Contact information
Gunton: kbgunton@comcast.net