Glaucoma: Complicated cases
September 2023
by Liz Hillman
Editorial Co-Director
When it comes to malignant glaucoma, why it occurs, its management, and if possible, its prevention, Matt Schlenker, MD, and Devesh Varma, MD, both think it’s important to first discuss some of the misunderstanding that has surrounded this topic.
The term “malignant glaucoma” was coined by Albert von Graefe in 1869 when he published a paper on acute angle closure glaucoma in patients after peripheral iridotomy, with shallowing of the anterior chamber and high intraocular pressure.1
Dr. Varma and Dr. Schlenker said there is a history of malignant glaucoma being described as aqueous misdirection. As Dr. Varma put it, “In the early days, malignant glaucoma was described as the shallowing of the peripheral and central anterior chamber with high pressure. People weren’t sure what the cause was. They thought maybe aqueous was going in the wrong direction and called it aqueous misdirection.”
Dr. Varma and Dr. Schlenker said this is not what’s happening. The seminal paper in 2009 by Harry Quigley, MD, cleared up what’s happening in these cases and began to change what Dr. Varma said is a misnomer.2 In the abstract of the paper, Dr. Quigley wrote:
When the pupil dilates, the iris typically decreases its volume by losing extracellular fluid. Eyes with angle-closure lose less iris volume with pupil dilation, contributing to obstruction of the trabecular meshwork. Expansion of choroidal volume is a dynamic phenomenon and is a major risk factor in angle-closure. The mechanism of malignant glaucoma seems likely to result from poor conductivity of fluid through the vitreous, and past suggestions that it results from “misdirected” aqueous are not consistent with physiological principles.
When malignant glaucoma can occur
There are a few clinical scenarios in which malignant glaucoma is more likely to occur. Dr. Schlenker said the most profound precipitating event is shallowing of the anterior chamber, for instance after filtering surgery, such as a trabeculectomy or tube shunt surgery in at-risk eyes. He said that any manipulation in the eye, even phacoemulsification, depending on other risk factors, can also result in malignant glaucoma. Female patients are more likely to have this occur, as are eyes with a small anterior chamber and a small axial length, according to Dr. Schlenker. He added that there is mounting evidence that zonulopathy is a risk factor for malignant glaucoma.
Dr. Varma said there is a risk for malignant glaucoma, in certain eyes, when anterior chamber shallowing occurs, for instance when you’re changing instruments in and out of the eye.
“It causes the choroid to swell, and in a small eye, there is not much space for that swelling, so it pushes everything forward,” he said. “In a small eye, the normal mechanisms to reset, to balance between the front chamber and the back chamber, don’t work as well, so you end up unable to reverse it. The eye can’t recalibrate, and it progressively pushes everything forward. The back chamber and the front chamber get out of balance.”
The physicians said that malignant glaucoma can occur intraoperatively or can develop over time postoperatively. Postoperatively, Dr. Varma said the lens will start to shift forward.
“At day 1 the patient could look good, but at week 1 they’re a –1 or –1.5 myope because the lens has shifted forward, then they could be –3 or –4 by the end of the month; … they come back unhappy because now they’re nearsighted even more. Progressive myopia is not an IOL calculation problem; one needs to look deeper,” Dr. Varma said.
Inas Aboobakar, MD, told EyeWorld that malignant glaucoma classically occurs in the early postop period after incisional glaucoma surgery in eyes with a history of angle closure, but she added that it can also be seen in predisposed eyes after cataract surgery, iridotomy, or when starting miotic therapy.
How to manage malignant glaucoma
If you see the chamber shallowing intraoperatively, the first thing to do is determine the cause. Dr. Schlenker said chamber shallowing that is not the result of malignant glaucoma includes leaky wounds, true fluid misdirection through impaired zonules to the posterior chamber, or a suprachoroidal hemorrhage. If the chamber is shallowing, one must address the underlying cause immediately. Check the wounds, and maintain the anterior chamber as much as possible. If the red reflex is dimmed and the fundus exam reveals evidence of a suprachoroidal hemorrhage, he would suture the wounds, form the anterior chamber, and defer any further surgery. If the problem is truly malignant glaucoma, you must consider doing an irido-zonulo-hyaloidotomy. “You need to create a conduit from the back of the eye to the front of the eye to establish an equilibrium; eliminate this pressure gradient between the front and the back of the eye. I usually do an anterior vitrectomy where I’ll do an anterior approach, unless the chamber is so profoundly shallow where I’d have to do a pars plana approach,” he said.
If malignant glaucoma develops postop, Dr. Varma said he’ll most often take the patient back to the OR and use the vitreous cutter, but he added that you could do a YAG laser iridotomy, going through the zonules and the hyaloid. Then you can go in with viscoelastic and push the lens back manually. Dr. Varma published a paper on the management of malignant glaucoma after cataract surgery, describing these techniques, in 2014.3
Dr. Schlenker said if malignant glaucoma occurs postop, he will start with atropine and likely aqueous suppression. This pulls the lens backward, and in some cases, if the patient has been on the drop for weeks to months and you can do a trial off it, as the system has been reset, they no longer need the atropine. Dr. Aboobakar’s initial management includes cycloplegics and aqueous suppressants, and she said hyperosmotic agents can be considered.
Dr. Aboobakar said she’ll consider either laser or surgical intervention in cases refractory to medical management. “In pseudophakic or aphakic patients, Nd:YAG laser can be applied in the clinic to disrupt the anterior vitreous face and allow aqueous to flow anteriorly. Surgical management with vitrectomy combined with irido-zonulo-hyaloidotomy provides definitive treatment in cases refractory to medical and/or laser therapy,” she said.
Prevention
From Dr. Aboobakar’s perspective, the underlying disease mechanisms are not yet fully understood, and methods for primary prevention of malignant glaucoma are not well studied.
“Once an individual has developed malignant glaucoma in one eye, prophylactic postoperative cycloplegia or vitrectomy at the time of cataract surgery in the contralateral eye can be considered, though the effectiveness of these measures has not been investigated with prospective studies to date,” she said.
Dr. Varma said the biggest preventative effort is to avoid a decompression event by maintaining anterior chamber pressurization when you’re changing instruments. In a small eye, Dr. Varma continued, you might do a prophylactic vitrectomy to make space, and use oral carbonic anhydrase inhibitors or mannitol ahead of time.
“That helps make space, but if you have a big decompression, it doesn’t matter if you’ve made space, you can still induce malignant glaucoma,” he said.
Dr. Schlenker said in eyes with an axial length less than 20 mm, he will consider doing a prophylactic irido-zonulo-hyaloidotomy when doing cataract surgery. He might also do this if a patient is at higher risk, such as if they had malignant glaucoma in their other eye.
Dr. Schlenker emphasized that early recognition of malignant glaucoma is important.
“The worst case scenario is someone who has subtle malignant glaucoma, their angles are closed, and it gets sat on for years, and they slowly develop scar tissue in their drainage system. By the time they get sent to me, their drainage system is completely closed off (peripheral anterior synechiae), and their eye pressure is really high,” he said.
“Retrospective case series suggest that most individuals with malignant glaucoma will go on to need vitrectomy combined with irido-zonulo-hyaloidotomy for definitive management,” Dr. Aboobakar said. “With prompt diagnosis and treatment, malignant glaucoma can resolve, though irreversible vision loss may occur depending on the duration and level of IOP elevation.”
ARTICLE SIDEBAR
A case example
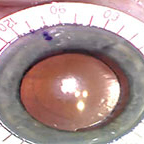
Dr. Aboobakar described a 78-year-old female with a history of laser peripheral iridotomy for acute angle closure attack in the left eye 15 years ago who underwent uncomplicated cataract surgery in this eye. She was doing well at her postop week 1 visit, with good visual acuity in the operative eye (20/25) and IOP 15 mm Hg. Three days later, however, she presented to the emergency room with acute onset headache, eye pain, blurry vision, and nausea/vomiting. The left eye visual acuity was 20/800, IOP was 48 mm Hg, the pupil was mid-dilated, the anterior chamber was diffusely shallow with irido-corneal touch in the periphery, and a patent peripheral iridotomy and posterior chamber intraocular lens were noted. B-scan ultrasound did not demonstrate choroidal effusions, suprachoroidal hemorrhage, or mass lesions. UBM showed anterior displacement of the lens-iris diaphragm and anterior rotation of the ciliary body.
The patient was started on maximal topical IOP lowering treatment, topical atropine, and oral acetazolamide with improvement in IOP to 28 mm Hg, though 2 days later IOP was again elevated to 45 mm Hg with anterior chamber shallowing. The patient underwent vitrectomy combined with irido- zonulo-hyaloidotomy with improvement in IOP to 11 mm Hg, deepening of the anterior chamber, and resolution of symptoms.
About the physicians
Inas F. Aboobakar, MD
Instructor in Ophthalmology
Massachusetts Eye and Ear/Harvard Medical School
Boston, Massachusetts
Matt Schlenker, MD
Associate Professor
University of Toronto
Toronto, Canada
Devesh Varma, MD
Assistant Professor of Ophthalmology
University of Toronto
Toronto, Canada
References
- von Graefe A. Beitrage zur pathologie und therapie des glaucoms. Archiv fur Ophthalmologie. 1869;15:108–252.
- Quigley HA. Angle-closure glaucoma—simpler answers to complex mechanisms: LXVI Edward Jackson Memorial Lecture. Am J Ophthalmol. 2009;148:657–669.
- Varma DK, et al. Malignant glaucoma after cataract surgery. J Cataract Refract Surg. 2014;40:1843–1849.
Relevant disclosures
Aboobakar: None
Schlenker: None
Varma: None
Contact
Aboobakar: inas_aboobakar@meei.harvard.edu
Schlenker: matt.schlenker@utoronto.ca
Varma: devesh.varma@prismeye.ca