Refractive
December 2020
by Liz Hillman
Editorial Co-Director
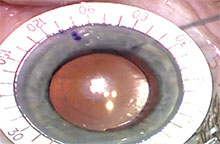
Source: John Berdahl, MD
Whether astigmatic correction was targeted in cataract surgery or not, there is always a risk for residual astigmatism postop. When to address this astigmatism—and how—depends on several factors, including patient perception, healing time, trust in measurements, and more.
John Berdahl, MD, Bryan Lee, MD, JD, Deborah Ristvedt, DO, Russell Swan, MD, and William Wiley, MD, continued their discussion with EyeWorld to round out the topic of astigmatism management in cataract surgery (see page 74).
The first thing to do when assessing for residual astigmatism is to make sure the cornea is well healed, which the doctors said is about 3–4 weeks postop. After that, you need to take the patient’s personality into account, Dr. Wiley said.
“Some patients come in with a diopter of astigmatism with the rule but they’re ecstatic … maybe in their eye the astigmatism is helping them,” he said. “If the patient is happy, I don’t care what the residual astigmatism is. I don’t want to fix what’s not broken.”
To Dr. Wiley, ophthalmologists should get used to thinking about it as “managing astigmatism” rather than “eliminating astigmatism.”
If a postop patient comes in and is symptomatic with residual astigmatism, it’s something that needs to be addressed.
“I tell patients there are three options: We can treat it surgically, we can treat it with glasses, or we can treat it with contact lenses,” Dr. Wiley said, noting that some patients are happy to have it treated with the latter two options.
“Some patients come in with a diopter of astigmatism with the rule but they’re ecstatic … maybe in their eye the astigmatism is helping them. If the patient is happy, I don’t care what the residual astigmatism is. I don’t want to fix what’s not broken.”
—William Wiley, MD
Those with their heart set on spectacle and contact lens independence have a few surgical options. Many of the doctors interviewed said they would use astigmatismfix.com, if they used a toric lens, to determine if the residual astigmatism could be corrected with a lens rotation. If not, then lens exchange or LASIK/PRK touchup could be needed.
“The surgery to use will depend on multiple factors, such as the time since surgery; the IOL type and the patient’s satisfaction with it; the patient’s preferred time frame for resolution; and intraoperative observations such as zonulopathy during phaco,” Dr. Lee said.
Dr. Wiley said if he’s going to do LASIK or PRK, he will perform a YAG capsulotomy first. He explained that if the patient were to get a refractive procedure and later develop PCO that required a YAG, the refractive prescription could change. Though he prefers to get the refraction to its most final point before treating, he cautioned that a YAG shouldn’t be taken lightly. If a patient has a multifocal lens and they’re not happy with the quality of vision due to the multifocality, you might want to avoid a YAG due to the difficulty of IOL exchange should one be needed in the future.
Dr. Ristvedt and Dr. Swan said they wait up to 3 months to get repeat measurements that are consistent before scheduling the patient for a LASIK fine tune.
How much residual astigmatism is impactful enough to correct? Dr. Wiley’s comment about patient perception comes into play here, but Dr. Berdahl said he and his team recently analyzed their data as they corrected low amounts of residual astigmatism (0.5–0.75 D) with LASIK and found it had a meaningful impact on patients’ visual acuity.
Dr. Swan emphasized the importance of following the entire optical path through the eye before taking corrective action, making sure that things like dryness, lens positioning, early PCO, or low-grade CME aren’t the cause of refractive error.
“Rule out all treatable causes and also rule out the potential untreatable causes that might be the real reason and don’t try to blame the astigmatism,” Dr. Wiley said.
About the doctors
John Berdahl, MD
Vance Thompson Vision
Sioux Falls, South Dakota
Bryan Lee, MD, JD
Altos Eye Physicians
Los Altos, California
Deborah Ristvedt, DO
Vance Thompson Vision
Alexandria, Minnesota
Russell Swan, MD
Vance Thompson Vision
Bozeman, Montana
William Wiley, MD
Cleveland Eye Clinic
Division of Midwest
Vision Partners
Relevant disclosures
Berdahl: Alcon, Bausch + Lomb, Johnson & Johnson Vision, RxSight
Lee: Carl Zeiss Meditec
Ristvedt: None
Swan: None
Wiley: Alcon, Johnson & Johnson Vision, RxSight, Carl Zeiss Meditec
Contact
Berdahl: john.berdahl@vancethompsonvision.com
Lee: bryan@bryanlee.pro
Ristvedt: deborah.ristvedt@vancethompsonvision.com
Swan: russell.swan@vancethompsonvision.com
Wiley: wiley@cle2020.com



