ASCRS News: EyeSustain Update
September 2022
by Aakriti G. Shukla, MD, and David F. Chang, MD

The healthcare sector is responsible for 10% of greenhouse gas emissions produced in the U.S.1 ORs and labor and delivery services produce 70% of medical waste. With 29 million cataract surgeries performed globally in 2019, procedural volumes in ophthalmology are the highest of any specialty.2 As ophthalmologists, we have the potential to make impactful change by informing policy and modifying wasteful practices. Most ophthalmologists are in agreement with this; a recent survey-based study with more than 1,000 respondents found that 93% of cataract surgeons think that approaches to reduce OR waste should be developed.3
| Intraoperative change | January–March 2020 (Baseline) (n=56,551) Group 1 | May–August 2020 (COVID-19) (n=29,011) Group 2 |
|---|---|---|
| Change 1 | 2 to 4 patients in same OR simultaneously | Only 1 patient in the OR at a time |
| Change 2 | The OR floor is cleaned every 3 hours. The OR table and other surfaces are cleaned with antiseptic at end of day. | OR table, floor, and surfaces are cleaned with antiseptic after every case. |
| Change 3 | Neither the surgeon nor the scrub nurse changed gowns or gloves in between cases. Alcohol/chlorhexidine was used to clean gloves between cases. | Double gloves for both surgeon and scrub nurse. Outer glove is changed after each case. |
| Change 4 | Patients wore their own clothing in the OR without wearing gowns. | Patients wore masks and laundered gowns over their clothing. |
| Cataract surgery type | January–March 2020 Group 1 | May–August 2020 Group 2 | Difference (95% CI) | P value | ||
|---|---|---|---|---|---|---|
| Number of surgeries | Number of POE (%) | Number of surgeries | Number of POE (%) | |||
| Phaco | 27,454 (49%) | 1 (0.003%) | 15,061 (52%) | 0 (0.00%) | 0.000036 (–0.000035 to 0.000107) | 0.46 |
| MSICS | 29,097 (51%) | 2 (0.006) | 13,950 (48%) | 2 (0.014%) | 0.00007 (–0.0001874 to 0.00033) | 0.45 |
| Total | 56,551 | 3 (0.005) | 29,011 | 2 (0.006%) | –0.000015 (–0.00013 to 0.00009) | 0.77 |
Source (all): Aakriti G. Shukla, MD, and David F. Chang, MD
The Aravind Eye Care System (AECS) is globally recognized for its forward-thinking eyecare models. This group of 14 regional eye hospitals in south India has consistently demonstrated delivery of safe, cost-effective, high-volume ophthalmic surgery with excellent outcomes.4,5 These accomplishments are accompanied by AECS’s focus on environmental and economic sustainability. Twenty cataract surgeries at AECS create the same level of carbon emissions as one cataract surgery in the U.K.6 More than 50% of surgeries performed at AECS are offered for free or at a steeply discounted price; despite this, the organization is consistently profitable.
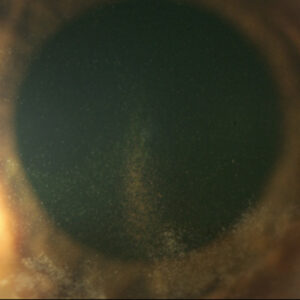
The British Journal of Ophthalmology recently published a study from our group, titled “Changing Operating Room Practices: The Effect on Postoperative Endophthalmitis Rates Following Cataract Surgery.”7 When AECS resumed surgery following the April 2020 pandemic lockdown, they adopted four new OR protocols designed to reduce the risk of COVID-19 transmission. This retrospective, sequential, clinical registry study analyzed whether these more stringent protocols, which are mandatory in the U.S., reduced Aravind’s rate of postoperative endophthalmitis following cataract surgery.
The study included consecutive patients who underwent cataract surgery at the Madurai regional AECS hospital during 2020. Two groups were compared; Group 1 underwent surgery prior to the institution of COVID-19 protocols (between January 1, 2020, and March 30, 2020) and Group 2 underwent surgery following the new protocol adoption (between May 1, 2020, and August 1, 2020). April 2020 was not included in the analysis because surgery was limited to emergency or non-elective procedures. Group 2’s time period was longer because of reduced surgical volume due to the pandemic. Outcome measures were the rate of postoperative endophthalmitis and complications such as posterior capsular rupture and zonular dialysis.
The four changes are described in Table 1. Aside from these modifications, the surgical and perioperative protocols were identical for the two groups. Postoperative outcomes are described in Table 2. A total of 85,562 cataract surgeries were included in the study, of which 56,551 surgeries were in Group 1, and 29,011 were in Group 2. The study found that 3 eyes (0.005%) in Group 1 and 2 eyes (0.006%) in Group 2 developed postoperative endophthalmitis (P=0.77). The endophthalmitis rate in this study is consistent with a prior study at AECS of 335,000 consecutive phacoemulsification cases (0.01%).4
“Importantly, despite having multiple patients in the room and reusing of surgical instruments, phacoemulsification tubing, and surgical gowns, postoperative endophthalmitis rates at AECS were lower than the rate reported in the U.S. by the Intelligent Research in Sight (IRIS) Registry.”
There was no difference in proportions of phacoemulsification and manual small incision surgery (MSICS) between the two groups, with Groups 1 and 2 having 29,097 (51%) and 12,950 (48%) MSICS cases and 27,454 (49%) and 15,061 (52%) phacoemulsification cases, respectively (P=0.77). The rates of posterior capsular rupture and zonular dialysis were <1.5%, without a difference between the two groups.
The study’s findings demonstrate that adopting the four Western OR protocols did not lower endophthalmitis rates following cataract surgery as compared to AECS’ standard protocols. Importantly, despite having multiple patients in the room and reusing of surgical instruments, phacoemulsification tubing, and surgical gowns, postoperative endophthalmitis rates at AECS (0.006%) were lower than the rate reported in the U.S. by the Intelligent Research in Sight (IRIS) Registry (0.04%).8
AECS regularly monitors intraoperative and postoperative surgical outcomes through its electronic clinical registry. By critically evaluating the impact of each step of its surgical protocols and the necessity of each item in the OR, AECS can offer cost-effective ophthalmic surgery without jeopardizing patient safety. Of note, all patients in this study received intracameral moxifloxacin prophylaxis. The findings from this study and others7,9,10 demonstrate the effectiveness of intracameral antibiotics even in the setting of routinely reusing supplies, medications, surgical devices, and OR attire.
In the U.S., we are strictly prohibited from reusing surgical gowns and gloves, or from having more than one patient in the operating room. The risk of microbial cross-contamination is considered high enough that repeatedly violating these policies would lead to closure of the surgical facility. Our study, involving more than 85,000 consecutive patients, found no difference in endophthalmitis rate with or without taking these precautions. This challenges the necessity of our zero-tolerance prohibition of these four OR policies routinely employed at AECS. Because of the substantial economic and environmental cost of needless surgical waste, we should continue to study other OR policies and regulations that may be unnecessary for ophthalmic surgery.
Editors’ note: Dr. Shukla is chair of the EyeSustain Editorial Board. Dr. Chang is chair of the EyeSustain Medical Advisory Board.
References
- Eckelman MJ, Sherman J. Environmental impacts of the U.S. health care system and effects on public health. PLoS One. 2016;11:e0157014.
- Freeman W. 2020 Cataract Surgical Equipment Market Report. 2020:55. Table 11. Market Scope. July 2020. Accessed April 15, 2021. staging.market-scope.com/files/products/brochures/196/2020%20Cataract%20Equipment%20Report%20Brochure.pdf
- Chang DF, Thiel CL, Ophthalmic Instrument Cleaning and Sterilization Task Force. Survey of cataract surgeons’ and nurses’ attitudes toward operating room waste. J Cataract Refract Surg. 2020;46:933–940.
- Haripriya A, et al. Endophthalmitis reduction with intracameral moxifloxacin in eyes with and without surgical complications: Results from 2 million consecutive cataract surgeries. J Cataract Refract Surg. 2019;45:1226–1233.
- Haripriya A, et al. Complication rates of phacoemulsification and manual small-incision cataract surgery at Aravind Eye Hospital. J Cataract Refract Surg. 2012;38:1360–1369.
- Thiel CL, et al. Cataract surgery and environmental sustainability: Waste and lifecycle assessment of phacoemulsification at a private healthcare facility. J Cataract Refract Surg. 2017;43:1391–1398.
- Haripriya A, et al. Changing operating room practices: the effect on postoperative endophthalmitis rates following cataract surgery. Br J Ophthalmol. 2022. Online ahead of print.
- Pershing S, et al. Endophthalmitis after cataract surgery in the United States: A report from the Intelligent Research in Sight Registry, 2013–2017. Ophthalmology. 2020;127:151–158.
- Ravindran RD, et al. Incidence of post-cataract endophthalmitis at Aravind Eye Hospital: outcomes of more than 42,000 consecutive cases using standardized sterilization and prophylaxis protocols. J Cataract Refract Surg. 2009;35:629–636.
- Haripriya A, et al. Endophthalmitis reduction with intracameral moxifloxacin prophylaxis: Analysis of 600000 surgeries. Ophthalmology. 2017;124:768–775.
Contact
Chang: dceye@earthlink.net
Shukla: ag2965@cumc.columbia.edu