Cataract
June 2022
by Ellen Stodola
Editorial Co-Director

Source: Nandini Venkateswaran, MD
Posterior capsule rupture (PCR) is one of the most dreaded complications for cataract surgeons. This complication will happen to every surgeon, no matter how great their skill, said Soroosh Behshad, MD.
Dr. Behshad, along with Zaina Al-Mohtaseb, MD, and Nandini Venkateswaran, MD, discussed PCR, when it can occur, how to reduce the risk, and techniques and IOL options that can be used.
Rates of PCR depend on level of experience and the complexity of the case, Dr. Behshad said, with rates varying between 1–14% of cases.1 When looking at a subset of surgeons who were more than 5 years out of training, these rates dropped to less than 5% of cases.2,3
Dr. Venkateswaran agreed that percentages of PCR may be variable, depending on surgeon experience. She estimated her rate is 1–2%. She noted that certain cases will lead to a higher risk of PCR. A dense cataract, a poorly dilating pupil (from medication use, prior trauma, chronic inflammation, or posterior synechiae), pseudoexfoliation, shallow anterior chamber, or high myopia all have very different anatomic circumstances that can increase the chance of a PCR, she said, noting that as a corneal specialist she is often doing cataract surgery on eyes with very sick, irregular, or scarred corneas, which can increase risk for PCR due to a poor surgical view. “Ultimately, I think good preoperative preparation helps reduce the risk of a PCR occurring,” she said. “You have to go in knowing there’s a higher risk for complications, and you have to take appropriate measures, whether it be changing the intracameral medications you’re using, using pupil expansion devices, changing phaco settings so you’re operating slower but more efficiently, using viscoelastic to protect the posterior capsule, or using alternative lighting to help improve illumination.”
“Ultimately, I think good preoperative preparation helps reduce the risk of a PCR occurring.”
Nandini Venkateswaran, MD
Dr. Al-Mohtaseb said there are a number of factors that can increase risk for tears or PCR. The first thing she noted was prior surgery, especially prior retinal surgery. Additionally, if there are any zonular loss issues due to trauma or systemic diseases like pseudoexfoliation, it can be a more complicated surgery. The presence of a posterior polar cataract or anything else that can cause the posterior capsule to not be normal are other scenarios that Dr. Al-Mohtaseb noted may increase the likelihood of PCR.
Posterior capsular tear or rupture can happen at any time during cataract surgery, Dr. Al-Mohtaseb stressed. Some might think this is just an issue when doing phacoemulsification, but she noted the importance of recognizing that it can happen at any time during a case.
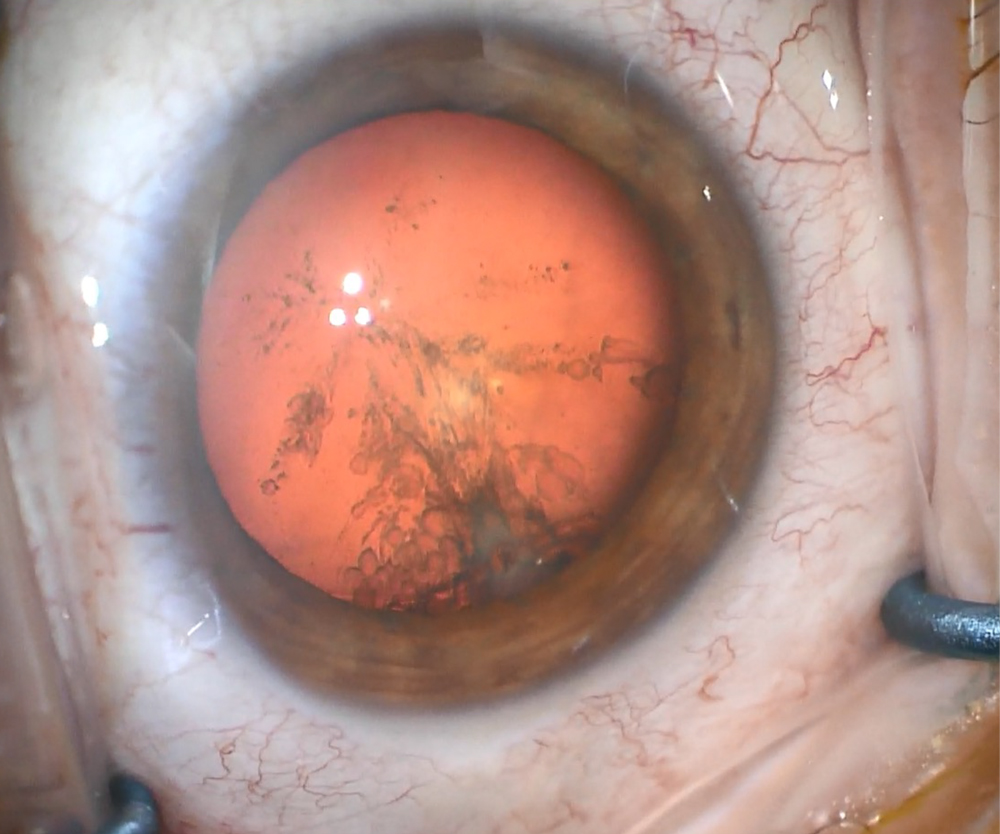
Dr. Behshad added that most risk factors that predispose cases to PCR can be identified preoperatively. Twenty-five percent of PCR is thought to be due to posterior polar cataracts, which can be identified on slit lamp exam or with ultrasound biomicroscopy.
It is important to not hydrodissect the nucleus in the setting of posterior polar cataracts. Instead consider gentle viscodelineation as this can help prevent extension of the capsular defect. It is key to identify any other preoperative risk factors that may increase risks for a PCR, such as small pupils, pseudoexfoliation, zonular weakness/loss from prior trauma, previous pars plana vitrectomy, and/or intravitreal injections, or a hypermature or black cataract. Care should also be taken ahead of time to prevent the case from progressing to a PCR. For example, in small pupils, consider iris expanding devices early and/or intracameral phenylephrine.
Dr. Behshad added that some other risk factors may be out of the surgeon’s hands, such as the patient’s involuntary movement during the surgery. In any patient where there is concern for poor cooperation during surgery, consider taping their head or using general anesthesia.
There are also surgeon or machine-related risk factors for PCR, he added. On the surgeon’s side, these include too much pressure when hydrodissecting, issues when chopping the nucleus, and using an unfamiliar machine or suboptimal machine settings. Care should be taken during nucleus disassembly and removal to prevent post-occlusion surge, a common cause for PCR during phacoemulsification.
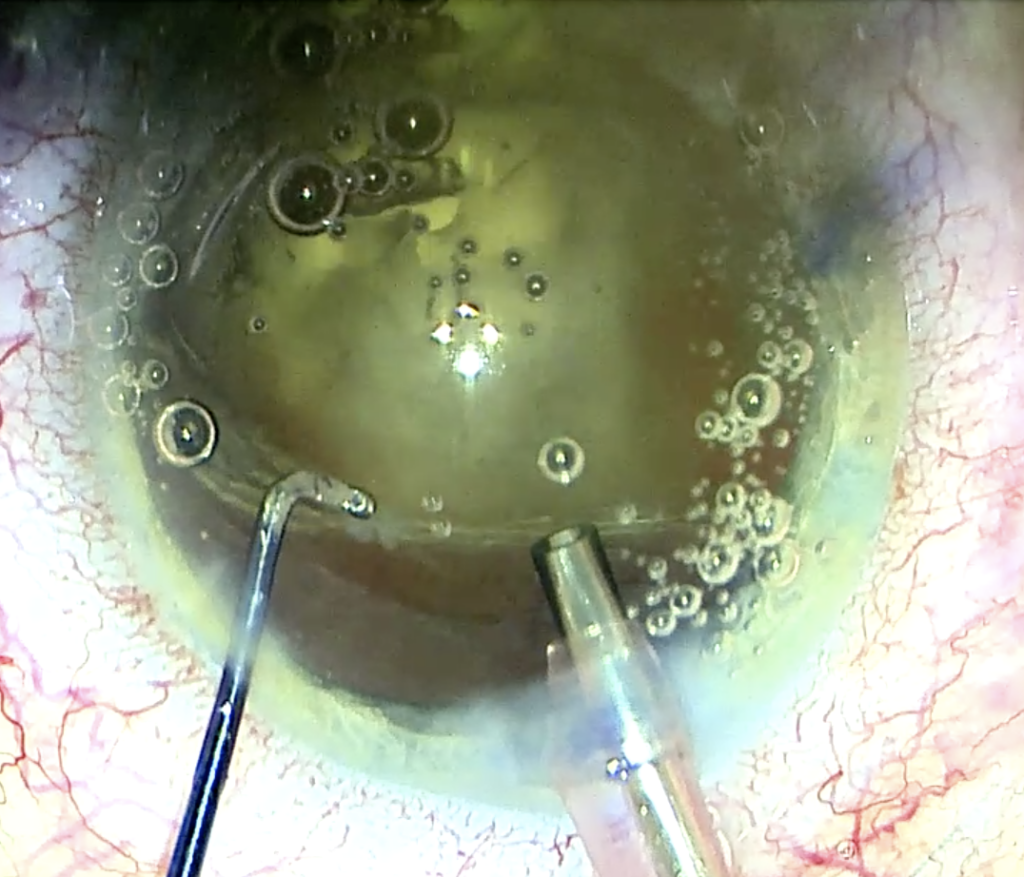
Source: Nandini Venkateswaran, MD
Techniques and IOL options
Dr. Al-Mohtaseb stressed that it’s not the end of the world if there is a posterior capsular tear. These patients can still do well. Early recognition is key because the surgeon wants to try to avoid postoperative complications, like decentration or subluxation of the lens, inflammation, cystoid macular edema, and macular tear or detachment.
The surgeon should use surgical techniques that avoid shallowing of the chamber, which means always placing OVD into the eye before removing the phaco tip or the I/A, Dr. Al-Mohtaseb said. At no point should the surgeon let the chamber shallow to prevent vitreous from prolapsing forward.
She also stressed the importance of doing a good anterior vitrectomy. She recommended a pars plana approach to the anterior vitrectomy, so the surgeon is bringing vitreous back and avoids traction. She uses triamcinolone to highlight any remnant vitreous in the anterior chamber and for its anti-inflammatory properties.
Dr. Venkateswaran noted that it’s important to assess how large the posterior capsular tear is, when in the case it occurred, and what the next steps are. “I think the best-case scenario is when there is a very small posterior rupture with no vitreous loss,” she said. “You may still be able to safely place a one-piece lens in the capsular bag.”
But if there is a large radial posterior capsular tear or an anterior capsular tear that extended posteriorly, the options are more limited, she said. She added that if there is an intact anterior capsule despite loss of a significant amount of the posterior capsule, the best option is to perform primary optic capture, where the surgeon places a three-piece lens in the sulcus space and tucks the optic of that lens underneath the anterior capsule. This technique provides a secure position for the IOL and reduces the likelihood of the lens moving around in the sulcus. The refractive outcome will also be comparable to placing the lens in the capsular bag. Sometimes there may not be enough of an anterior capsule to safely perform optic capture. If the surgeon is in doubt of the lens stability in the sulcus, he or she could place a suture to secure the haptics of the lens to the iris for additional support.
Dr. Venkateswaran noted that some surgeons, in cases where the PCR is small and central, will create a primary posterior capsulorhexis and perform posterior optic capture, where the IOL is placed in the bag and the optic is captured in the posterior capsulorhexis. This provides additional stability for the IOL, but it’s also tricky and will only work if a truly round posterior capsulorhexis can be made out of a small PCR; it will not work if there is a large radial PCR.
Source: Soroosh Behshad, MD, MPH

Source: Soroosh Behshad, MD, MPH
Dr. Venkateswaran also mentioned reverse optic capture, which she said can be useful if there is a PCR particularly in the setting of a premium lens. This could provide the patient the opportunity to still get the premium technology they want in a safe way.
Ultimately, these lenses, when optic captured, are extremely stable, Dr. Venkateswaran said. “I think there are issues when a surgeon places a three-piece lens in the sulcus, and they’ve lost a large portion of the anterior capsule. These lenses can move around quite a bit and can potentially dislocate, and that’s why fixating these lenses to the iris is a more stable option.” If the surgeon doesn’t think there is enough support for a three-piece in the sulcus, Dr. Venkateswaran recommended either putting an anterior chamber lens in or staging the procedure and coming back when the eye is quieter to perform a secondary lens fixation.
Dr. Behshad said that timing of the PCR and residual capsular strength is what will help determine IOL placement. “When there is a stable residual anterior capsule remaining, placement of a three-piece IOL in the ciliary sulcus would be the most acceptable option,” he said. “Reverse optic capture can be performed in this scenario to provide further IOL stability, but if the anterior capsulotomy is too small or large, it may not be possible in all cases.”
He said that if the PCR occurs after placement of a one-piece in the capsular bag, and the posterior rent or tear is stable with an intact anterior capsule, optic capture with the anterior capsule can be performed. Care and time should be taken to ensure that the IOL is stable in this configuration. “If there is any concern for stability, the one-piece IOL should be removed and a three-piece placed in the ciliary sulcus,” he said. “It is never OK to place a one-piece IOL in the ciliary sulcus, as this will lead to UGH syndrome.”
Placement of an ACIOL has been shown to lead to complications down the line, including glaucoma and corneal decompensation. Therefore, it may not be the best long-term option for patients, Dr. Behshad said, adding that other IOL placement techniques are dependent on surgeon skills. These techniques include suturing a three-piece IOL to the iris, suturing a three-piece IOL or PMMA IOL to the sclera, or intrascleral IOL fixation using a three-piece IOL with haptics made of polyvinylidene fluoride, such as the CT LUCIA 602 (Carl Zeiss Meditec).
Following IOL placement, care should be taken to do a complete anterior vitrectomy to ensure all prolapsed vitreous is removed from the anterior chamber, Dr. Behshad said. Dilute triamcinolone or acetylcholine should be considered to help identifying prolapsed vitreous, and the surgical approach, whether anterior or posterior, should be based on surgeon experience.
Dr. Al-Mohtaseb also highlighted lens options that are available if a posterior capsular tear or rupture does occur. Typically, if there is a small, circular tear that is centrally located, the surgeon could still do a one-piece in the bag, but for most posterior capsular tears, you typically want to put a three-piece lens in the sulcus.
“I’m a firm believer that you need to also optic capture that three-piece lens to avoid decentration in the future and UGH syndrome, especially in patients with long axial lengths,” Dr. Al-Mohtaseb said. “I don’t like putting three-piece lenses in the sulcus without optic capture.” Another benefit of doing optic capture is the surgeon doesn’t have to change the power of the IOL because the position of the IOL is theoretically the same as if they’d put a one-piece lens in.
Additionally, if the anterior capsule is too large or the surgeon can’t get a good optic capture, Dr. Al-Mohtaseb said she likes to make the posterior capsular tear round and circular and capture the lens into the posterior capsulotomy.
In a complex case where there is a large posterior capsular tear, zonular loss, etc., Dr. Al-Mohtaseb said surgeons might want to choose another technique, like getting rid of the capsule altogether and doing Yamane intrascleral fixation.
Dr. Behshad added that in cases where the surgeon is planning for astigmatism management with a toric IOL, there currently are no toric IOL options FDA approved for placement in the ciliary sulcus. There has been some movement in developing a toric IOL that is stable in the sulcus and not a one-piece IOL, but currently none are available in the U.S., he said, adding that astigmatism management can be completed with placement of corneal LRIs or subsequent laser vision correction.
Both Drs. Al-Mohtaseb and Behshad again stressed the importance of early recognition of PCR and having a plan in place if it occurs.
They said to not chase lens material that falls posteriorly. Dr. Al-Mohtaseb said that this can potentially cause traction or retinal tears. Dr. Behshad added that in this case, risks increase exponentially for retinal damage that can lead to permanent vision loss. Remove as much of the cataract that is present anteriorly and complete a thorough vitrectomy, he said. If possible, place a three-piece IOL in the sulcus, and if there are retina services available, consider same-day lens fragment removal by a retina colleague. Otherwise, plan to involve retina early in the postop course.
About the physicians
Zaina Al-Mohtaseb, MD
Associate Professor
Baylor College of Medicine
Houston, Texas
Soroosh Behshad, MD, MPH
Associate Professor of Cataract, Corneal, and Refractive Surgery
Emory University School of Medicine
Atlanta, Georgia
Nandini Venkateswaran, MD
Cornea, Cataract, and Refractive Surgeon
Massachusetts Eye and Ear, Waltham
Waltham, Massachusetts
References
- Chakrabarti A, Nazm N. Posterior capsular rent: Prevention and management. Indian J Ophthalmol. 2017;65:1359–1369.
- Vajpayee RB, et al. Management of posterior capsule tears. Surv Ophthalmol. 2001;45:473–488.
- Greenberg PB, et al. Prevalence and predictors of ocular complications associated with cataract surgery in United States veterans. Ophthalmology. 2011;118:507–514.
Relevant disclosures
Al-Mohtaseb: None
Behshad: None
Venkateswaran: None
Contact
Al-Mohtaseb: zaina1225@gmail.com
Behshad: soroosh.behshad@emory.edu
Venkateswaran: nandini_venkateswaran@meei.harvard.edu



