ASCRS News: ASCRS/EyeWorld Journal Club
July 2021
by Sabrina Mukhtar, MD, Ian Conner, MD, and Evan Waxman, MD

Residency Program Director
University of Pittsburgh
Pittsburgh, Pennsylvania
In eyes that lack posterior capsular support, there are several methods to implant intraocular lenses, including iris-fixated IOLs,1 anterior chamber IOLs, and transscleral fixated IOLs.2–4 While sutured scleral fixated IOLs have been used historically, their limitations include prolonged surgical time, suture-induced inflammation, suture degradation, and long-term IOL subluxation or dislocation.5 In 1997, a sutureless transscleral fixation technique designed for posterior chamber IOLs was introduced by Maggi and Maggi.6 In 2007, intrascleral haptic fixation was suggested by Gabor et al.,7 followed by the introduction of the glued IOL technique by Agarwal in 2008.5 The glued IOL technique has undergone several modifications to give stability to the haptics and broaden its surgical indications.8–10 While short-term data was available, long-term outcomes data was absent from the literature, and this publication aimed to describe long-term functional and anatomical outcomes in eyes that underwent the glued IOL implantation technique.
Summary

Associate Residency
Program Director
University of Pittsburgh
Pittsburgh, Pennsylvania
This retrospective case series aimed to report the results and complications of glued transscleral fixated intraocular lenses over a 6- to 12-year period from a single institution. All surgeries were performed using the glued IOL technique as previously published.5,9,10 These patients were looked at by a single examiner, and all patients received standard postoperative care. Both anatomical and functional outcomes were measured including IOL positioning, scleral haptic visibility, iris and pupil anatomy, anterior chamber reaction, visual acuity, intraocular pressure, corneal endothelial density, corneal topography and keratometry, complications, and quality of life metrics (Visual Function Index-14 scoring system). Additionally, a scleral haptic visibility grading system was introduced, describing scleral flap thinning and haptic visualization at long-term follow-up.
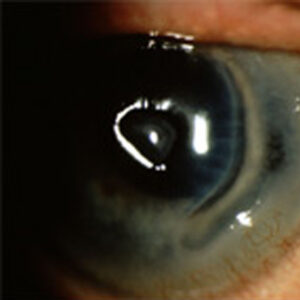
In this study, 91 eyes of 63 patients were included. The mean follow-up was 8.2 years. IOL position was measured by slit lamp biomicroscopy and anterior segment OCT. In this cohort, 5 eyes had clinically detectable mild IOL decentration at the slit lamp, two eyes showed pseudophacodonesis, four eyes had clinically detectable tilt, and 17 eyes showed optic microtilt on OCT. There was IOL-iris touch near the pupillary plane in 21 eyes on anterior segment OCT. Additionally, using the new haptic visibility grading system, the majority of cases were described as grade 0 or 1 showing no or minimal haptic visibility through the scleroconjunctiva.

Ophthalmology Resident
University of Pittsburgh
Pittsburgh, Pennsylvania
With regard to visual acuity, there was a significant improvement in uncorrected distance visual acuity postoperatively and no significant difference found in corrected distance visual acuity. Intragroup analysis in relation to age stratification showed no difference in mean corrected distance visual acuity. The mean postoperative refraction as represented in spherical equivalent was –1.1 D, and the mean ocular residual astigmatism was 1.1 D as determined using the Alpins method of vector analysis. Loss of corrected distance visual acuity was attributed to retinal detachment (n=2), traumatic optic neuropathy (n=1), and corneal decompensation (n=2). The mean postoperative intraocular pressure was significantly higher compared to preoperative IOP (p=0.001), and 10 eyes had an IOP of greater than 21 mm Hg, seven of which were diagnosed with glaucoma. One eye was documented to have uveitis-glaucoma-hyphema syndrome.
Additional complications noted in the postoperative period included corneal endothelial decompensation (n=3) at 5.3±3.5 years, cystoid macular edema (n=4), retinal detachment (n=3) at 2.6 years from surgery, and haptic subluxation (n=4) at 8±1.6 years postoperatively. In this cohort, secondary surgeries included penetrating keratoplasty (n=1), trabeculectomy (n=1), glaucoma drainage device insertion (n=1), haptic repositioning (n=3), IOL explantation (n=1), pupilloplasty (n=2), and retinal detachment repair (n=3). No eyes developed IOL dislocation, choroidal detachment, or endophthalmitis.
Discussion
The authors presented long-term results of the glued IOL technique that overall had good anatomical and functional outcomes showing stability in these complex patients.
It is imperative to have several techniques in one’s surgical repertoire to manage complex eyes with deficient capsules. Common indications for this technique include intraoperative posterior capsule rupture, subluxated cataract or IOL, aphakia, and ectopia lentis with deficient zonular fibers.11 When comparing the glued IOL technique to primary AC IOLs, transscleral fixated sutured IOLs, and iris claw IOLs, the authors reported less incidence of endothelial cell damage, retinal detachments, glaucoma, uveitis, macular edema, suture degradation, and IOL tilt12 and overall better outcomes.11,12 There is limited long-term data on current scleral fixated lens techniques, therefore this publication not only provides necessary data but is reassuring that overall, the glued IOL technique has a good long-term safety profile.
There are some considerations that should be made when using the glued IOL technique. The technique requires dissection of scleral flaps with a conjunctival cutdown, so it is not ideal in patients with conjunctival scarring, history of previous glaucoma surgeries, or history of vitreoretinal surgeries including scleral buckles. Additionally, the technique should be used with caution in eyes with compromised scleral integrity as sclerotomies are necessary to externalize the haptics. Patients with a history of uveitis have been shown to have higher incidence of cystoid macular edema and a longer time to resolution of anterior chamber inflammation compared to non-uveitic eyes undergoing the glued IOL technique.13 In short eyes, patients may be more likely to have haptic extrusion, resulting in a posteriorly positioned optic. On the other hand, in myopic eyes, it may be more difficult to perform the scleral tuck of the haptics given the larger limbus size.
When comparing outcomes of the glued IOL technique to the Yamane technique,14 IOL tilt in the glued IOL technique was reported to be less (0.8±1.7 degrees in the 90 to 270 axis and 0.4±1.2 degrees in the 0 to 180 axis versus mean 2.4 degrees in the Yamane technique).11,14 This is likely due to the fact that the scleral passage with the Yamane technique is more difficult, and the glued IOL technique uses bigger openings and allows for more consistent scleral passages, therefore, a surgeon may have more tilt with the Yamane technique when first learning it. Lens availability can also determine which technique to use; if the correct lens is unavailable to perform the Yamane technique, the glued IOL technique becomes a better option. Regardless, it is important to understand that both techniques have a role and surgeons should be skilled in both. More long-term outcomes data is needed comparing both sutureless transscleral fixated IOL techniques.
A few pearls mentioned by the panelists in the ASCRS Journal Club included performing a pars plana vitrectomy as there is a lot of posterior manipulation, especially at the vitreous base. Additionally, when a novice surgeon learns the technique, it would be helpful to use a lens with stronger haptics such as the CT Lucia 602 (Carl Zeiss Meditec), as there can be a lot of manipulation and torquing of the haptics earlier on. The surgeon should be mindful that the change in direction from the vertical sclerotomy to the horizontal scleral tunnel is a difficult angle and requires targeted manipulation of the haptics. Lastly, having an able assistant to hold the leading haptic during the handshake technique is important and should be considered during surgical planning.
In conclusion, the authors presented long-term results of the glued IOL technique that overall had good anatomical and functional outcomes showing stability in these complex patients. While there can be a steep learning curve associated with the technique, it is an important skill for a surgeon to have in their armamentarium for eyes with deficient capsules.
Glued intraocular lens in eyes with deficient capsules: A retrospective analysis of long-term effects
Dhivya Ashok Kumar, MD, FRCS, Amar Agarwal, MS, FRCS, Atul Dhawan, MBBS, MS, Vijayanand Thambusamy, MBBS, DO, Soundari Sivangnanam, DO, DNB, Triveni Venktesh, MBBS, MS, Radhika Chandrasekar, BSc
J Cataract Refract Surg. 2021;47(4):496–503.
- Purpose: To assess the long-term (6–12 years) results and complications of glued transscleral fixated intraocular lens (IOL).
- Setting: Dr. Agarwal’s Eye Hospital, Chennai, India.
- Design: Retrospective case series.
- Methods: Eyes with glued IOL with more than 5 years of follow-up were evaluated. Visual acuity (logMAR), IOL tilt, corneal topography, corneal endothelial cell density, intraocular pressure, central corneal thickness (CCT), central foveal thickness (CFT), and ocular residual astigmatism (ORA) were evaluated.
- Results: Overall, 91 eyes (63 patients) with mean postoperative 8.2±2.3 years were analyzed. The durations were 10–12 years in 31 (34%) eyes, 9 years in 14 eyes (15.3%) and 6–9 years in 46 eyes (50.5%), respectively. No subscleral haptic was visible in 50% of eyes. Mild, moderate, and severe grade of haptic visibility was noted in 33.5%, 9.4%, and 7%, respectively. The BCVA was 0.50±0.50 logMAR. Clinically no tilt was seen in 87 eyes (95.6%), while detectable tilt was seen in 4 eyes (4.3%). The OCT microtilt was 0.8±1.70 and 0.4±1.20 degrees in 90- and 180-degree axes, respectively. The mean iris vault was 0.45 mm, and the mean ORA was 1.1±1 D. Complications were glaucoma (7.6%), IOL luxation (4.4%), retinal detachment (3.2%), macular edema (4.3%), corneal decompensation (3.2%), uveitis (2.1%) and uveitis-glaucoma-hyphema syndrome (1%). Haptic reposition (3.2%), retinal detachment surgery (3.2%), keratoplasty (1%), pupilloplasty (2.1%), and IOL explantation (1%) were the second surgeries.
- Conclusion: Glued IOL has shown good anatomical and functional stability with minimal incidence of vision-threatening complications on long term.
ARTICLE SIDEBAR
The ASCRS Journal Club is a virtual, complimentary CME offering exclusive to ASCRS members that brings the experience of a lively discussion of two current articles from the Journal of Cataract & Refractive Surgery to the viewer. Co-moderated by Nick Mamalis, MD, and Leela Raju, MD, the April session featured a presentation by Kerry Solomon, MD, co-author of “Cataract surgery after myopic laser in situ keratomileusis: objective analysis to determine best formula and keratometry to use.” The second manuscript, “Glued intraocular lens in eyes with deficient capsules: retrospective analysis of long-term effects” was presented by Sabrina Mukhtar, MD, ophthalmology resident, University of Pittsburgh. To view the April Journal Club session, visit ascrs.org/clinical-education/journal-club/schedule/april-2021.
References
- Zeh WG, Price Jr FW. Iris fixation of posterior chamber intraocular lenses. J Cataract Refract Surg. 2000;26:1028–1034.
- Bleckmann H, Kaczmarek U. Functional results of posterior chamber lens implantation with scleral fixation. J Cataract Refract Surg. 1994;20:321–326.
- Koh HJ, et al. Scleral fixation technique using 2 corneal tunnels for a dislocated intraocular lens. J Cataract Refract Surg. 2000;26:1439–1441.
- OH H-S, et al. Surgical technique for suture fixation of a single-piece hydrophilic acrylic intraocular lens in the absence of capsule support. J Cataract Refract Surg. 2007;33:962–965.
- Agarwal A, et al. Fibrin glue-assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J Cataract Refract Surg. 2008;34:1433–1438.
- Maggi R, Maggi C. Sutureless scleral fixation of intraocular lenses. J Cataract Refract Surg. 1997;23:1289–1294.
- Gabor SGB, Pavlidis MM. Sutureless intrascleral posterior chamber intraocular lens fixation. J Cataract Refract Surg. 2007;33:1851–1854.
- Kumar DA, et al. Glued intrascleral fixation of posterior chamber intraocular lens in children. Am J Ophthalmol. 2012;153:594–601.
- Kumar DA, Agarwal A. Glued intraocular lens: a major review on surgical technique and results. Curr Opin Ophthalmol. 2013;24:21–29.
- Kumar DA, et al. Complications and visual outcomes after glued foldable intraocular lens implantation in eyes with inadequate capsules. J Cataract Refract Surg. 2013;39:1211–1218.
- Kumar DA, et al. Glued intraocular lens in eyes with deficient capsules: retrospective analysis of long-term effects. J Cataract Refract Surg. 2021;47:496–503.
- Wagoner MD, et al. Intraocular lens implantation in the absence of capsular support: a report by the American Academy of Ophthalmology. Ophthalmology. 2003;110:840–859.
- Kumar DA, et al. Uveitis and deficient lens capsules: Effect of glued intraocular lens on the visual outcome and the reactivation of inflammation. Indian J Ophthalmol. 2019;67:1610–1616.
- Yamane S, et al. Sutureless 27-gauge needle-guided intrascleral intraocular lens implantation with lamellar scleral dissection. Ophthalmology. 2014;121:61–66.
Contact
Mukhtar: mukhtars@upmc.edu
Waxman: waxmane@upmc.edu