Cornea
Spring 2024
by Ellen Stodola
Editorial Co-Director
Peripheral ulcerative keratitis (PUK) is an inflammatory condition that typically affects the peripheral cornea leading to corneal thinning and corneal melt. According to Ashraf Ahmad, MD, it affects around three patients per million per year. It is commonly associated with an underlying autoimmune process, such as rheumatoid arthritis, systemic lupus, inflammatory bowel disease, or ANCA vasculitides, among others, he said.
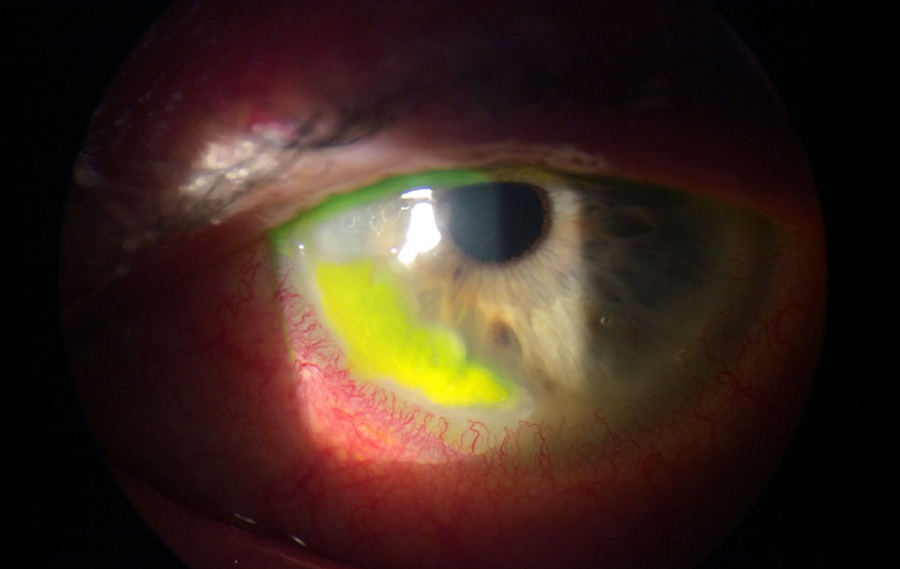
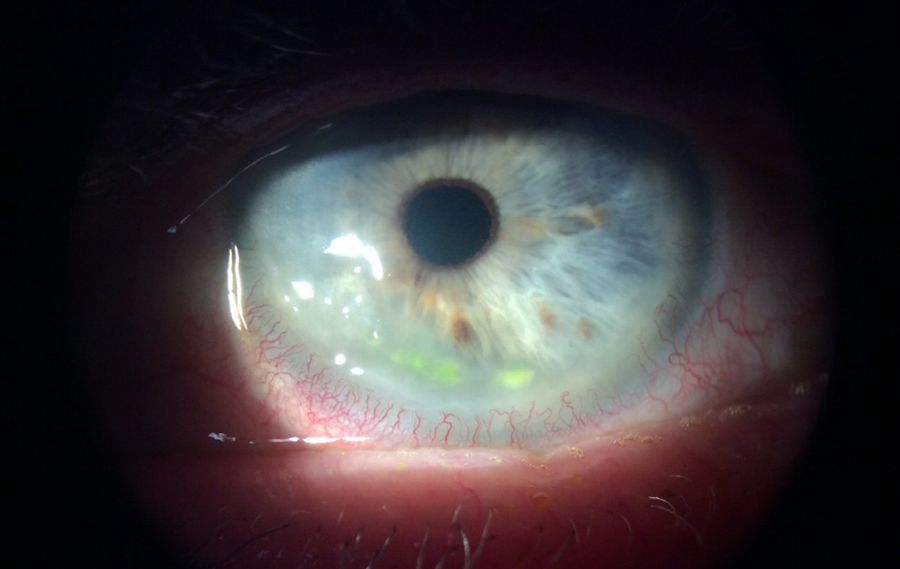
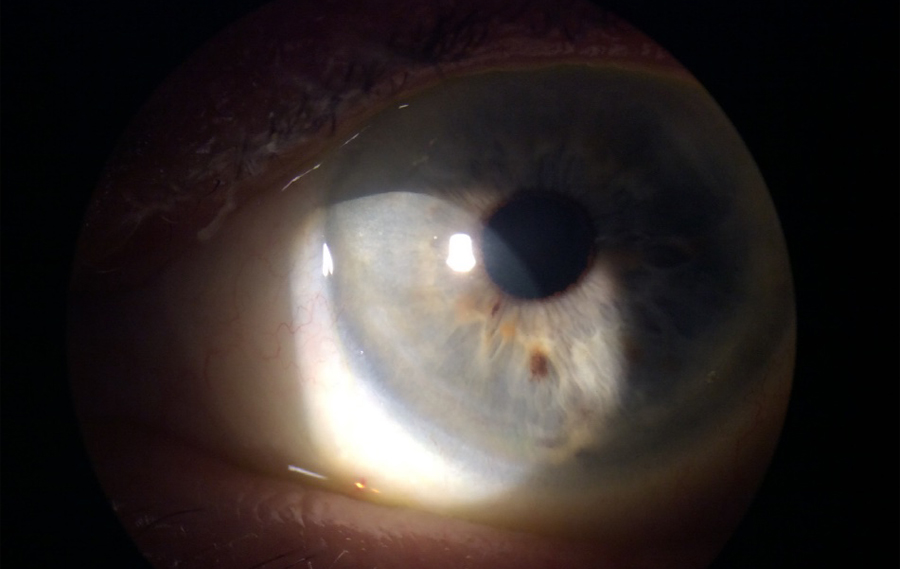
PUK is a clinical diagnosis, said Sanjay Kedhar, MD. “Patients may present with pain, redness, tearing, photophobia, or changes in vision. Slit lamp exam typically reveals a crescentic epithelial defect with stromal thinning in the peripheral cornea.” He added that in severe cases, the patient may present with a descemetocele or frank perforation of the cornea due to progressive stromal destruction and thinning. About a third of these patients will also have a concurrent scleritis.
“Slit lamp exam is imperative, as this is primarily a clinical diagnosis,” Dr. Ahmad said. “Exam will show a peripheral infiltrate adjacent to the limbus, often crescent shaped, with an overlying epithelial defect. Patient presentations can range from barely symptomatic to severe eye pain, redness, photophobia, and irritation.”
Since PUK is typically associated with an underlying autoimmune condition, Dr. Ahmad said an appropriate review of systems should be done followed by a targeted lab workup looking for autoimmune, rheumatic, and infectious causes. Corneal culture should be considered prior to initiating antibiotics to rule out the possibility of infectious keratitis.
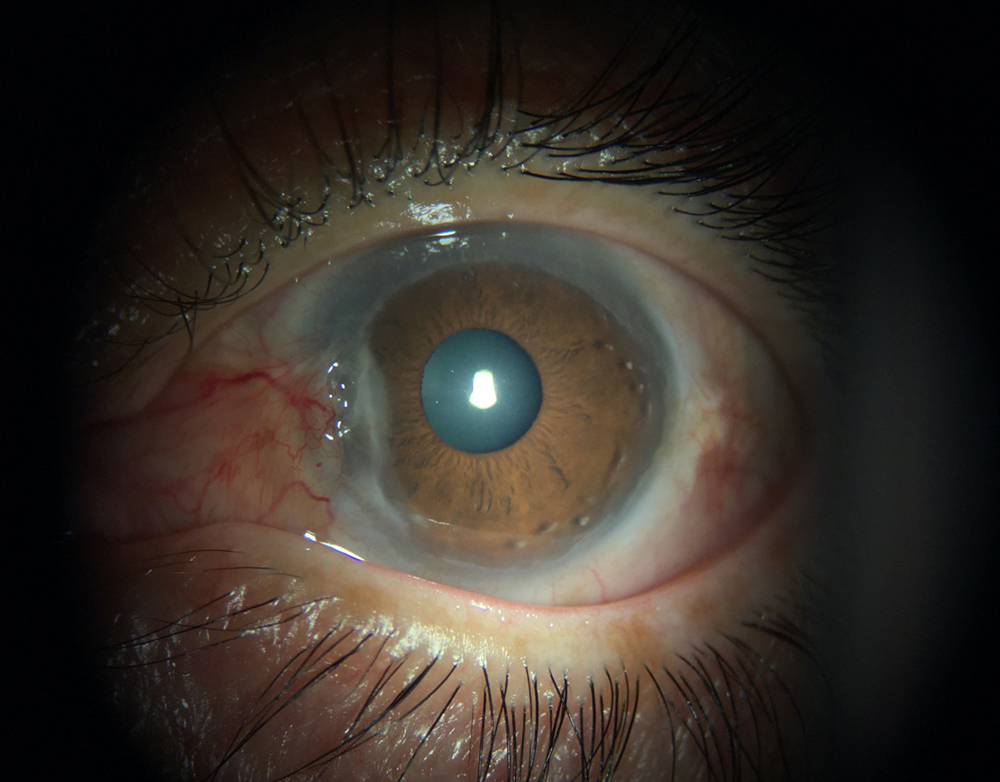
Source: Sanjay Kedhar, MD

Source: Sanjay Kedhar, MD
“A thorough history and physical exam is a key component of the workup,” Dr. Kedhar said. “Cultures from the bed of the lesion should be performed if an infection is suspected. Otherwise, laboratory testing should include a complete blood count, comprehensive metabolic panel, ANCA testing, urinalysis with microscopic analysis, syphilis testing, and a chest X-ray. Additional testing such as hepatitis B triple panel test, hepatitis C antibody, TB, corneal cultures, anti-CCP, rheumatoid factor, and ANA may be ordered based on patient history and risk factors.”
He added that there is a broad differential diagnosis for PUK, including corneal degenerations such as Terrien’s marginal degeneration, Fuchs superficial marginal keratitis, and pellucid marginal degeneration, as well as neoplastic etiologies such as carcinoma in situ.
Dr. Ahmad said there may be some challenges with confirming a diagnosis because many other conditions can mimic PUK. He expanded on the differential diagnosis to also include infectious keratitis, herpes viral keratitis, and staph marginal keratitis. “Differentiating between these entities can be challenging and requires a careful history and physical exam,” he said.
To treat PUK, Dr. Ahmad said patients typically require systemic steroids to control the local inflammation. “Topical steroids can be employed but often do not totally control the condition. They should be used judiciously, as they can promote further corneal thinning. Topical prophylaxis with antibiotics is important to prevent bacterial superinfection,” he said. “Additionally, oral doxycycline and vitamin C can help prevent corneal thinning by inhibiting matrix metalloproteinase activity and promoting collagen synthesis, respectively. Ultimately, many patients will need to bridge to steroid-sparing therapy for long-term control of PUK.” Dr. Ahmad added that comanagement with rheumatology is necessary for many of these patients.
Source: Ashraf Ahmad, MD
According to Dr. Ahmad, PUK flare-ups can resolve with treatment, however, recurrence is common, particularly if the underlying condition is not well controlled. With each recurrence, there is risk of corneal melt, perforation, scaring, and irregular astigmatism, which can lead to permanent loss of vision.
Dr. Ahmad added that approximately one-third of patients have an associated scleritis on presentation. It is important to evaluate for this and consider a B-scan if posterior scleritis is suspected.
Dr. Kedhar said that treatment of PUK will be based on the nature of the underlying disease. For autoimmune disorders, treatment consists of local and systemic treatment. Local therapy includes aggressive lubrication of the eye with preservative-free artificial tears and punctal occlusion to promote epithelial healing as well as oral doxycycline and vitamin C. Cyanoacrylate glue can be useful in cases of more severe thinning to limit ulceration. The conjunctiva in the area of inflammation can be recessed, and cyanoacrylate or amniotic membrane can be placed in the defect to limit inflammation and tissue destruction.
“Oral steroids are preferred over topical steroids due to increased risk of keratolysis with topical administration,” Dr. Kedhar said. “Oral steroids should be used aggressively at high doses initially to reduce tissue loss. In severe cases, patients with rheumatoid arthritis or disease that is not completely responsive to steroids or poorly controlled diabetics, systemic immunosuppression should be considered. A variety of agents can be used including methotrexate, mycophenolate mofetil, azathioprine tacrolimus, cyclophosphamide, chlorambucil, adalimumab, infliximab, or rituximab.”
Dr. Kedhar said that treatment should be geared toward arresting ongoing tissue destruction and inflammation. Even with adequate treatment, the areas of corneal thinning will remain. Depending on the amount of residual tissue left, surgical procedures can be tailored toward reinforcing any areas of weakness, he said. It can recur, especially if any underlying disease is not treated adequately. The epithelial defect should heal completely with appropriate treatment.
“Corneal stromal thinning generally does not reverse with medical treatment, but progression should stop. If the corneal thinning is excessive or there is perforation, surgical intervention including corneal patch grafts, crescentic keratoplasty, or corneoscleral procedures can be considered,” he said.
Dr. Kedhar said that ophthalmologists should be vigilant to rule out systemic disease or infection.
About the physicians
Ashraf Ahmad, MD
Cataract, Cornea & Refractive Surgery
Harvard Eye Associates
Laguna Hills, California
Sanjay Kedhar, MD
Clinical Professor of Ophthalmology
Gavin Herbert Eye Institute
University of California, Irvine
Irvine, California
Relevant disclosures
Ahmad: None
Kedhar: None
Contact
Ahmad: aahmad@harvardeye.com
Kedhar: skedhar@hs.uci.edu