ASCRS News: ASCRS/EyeWorld Journal Club
April 2022
by Tyler Friske, MD, Jacob Warmath, MD, and David Jackson, MD

Residency Program Director
Dean McGee Eye Institute
Oklahoma City, Oklahoma
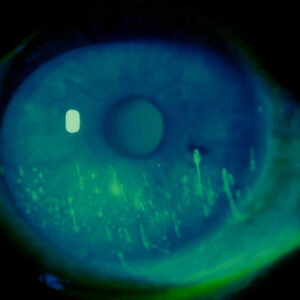
Small incision lenticule extraction (SMILE) is a corneal refractive procedure involving the use of a femtosecond laser to create an intrastromal corneal lenticule that is manually extracted as a single piece through a small incision. The precursor to modern SMILE was first described by Ito et al. in 1996.1 With the introduction of the VisuMax femtosecond laser (Carl Zeiss Meditec) in 2007, safety and efficacy results of femtosecond lenticule extraction were first reported by Sekundo et al.2 Following the development of femtosecond lenticule extraction, SMILE was developed to eliminate the need for flap creation. The first prospective studies of SMILE were reported in 2011.3–5 SMILE was approved for spherical myopic corrections by the FDA in the U.S. in 2016 and for compound myopic astigmatism in 2018.6
SMILE was first performed at a U.S. military-specific refractive surgery center in 2017. Sia et al. reported 1-year retrospective data noting vision outcomes similar to PRK and LASIK in addition to possible improvements in speed of visual recovery and predictability of visual outcomes.7 However, prior to the study reviewed in this article, there were no prospective military studies of SMILE to aid in establishing guidelines for U.S. military service members.
The purpose of this study was to evaluate early clinical, patient-reported, and profession- specific outcomes of SMILE in active duty U.S. military service members.

Resident
Dean McGee Eye Institute
Oklahoma City, Oklahoma
Design and methods
This prospective, single-center observational study included 74 eyes of 37 patients who underwent SMILE at the Warfighter Refractive Eye Surgery Program & Research Center and Night Vision and Electronic Sensors Directorate in Fort Belvoir, Virginia. Inclusion criteria included active duty U.S. military service members 22 years or older with manifest refractions within the FDA-approved parameters for SMILE and a stable refraction for at least 1 year. Exclusion criteria included pregnant or nursing patients, patients with an active or recurrent ocular disease or corneal abnormalities, and patients with a history of prior ocular surgery, eye trauma, or medical conditions that could impact postoperative healing.
The SMILE procedure was performed by two experienced surgeons. The laser parameters and surgical technique were standardized. Patients underwent a comprehensive preoperative screening examination. Patients were then examined postoperatively at 1 and 7 days, in addition to 1 month and 3 months.
Outcome measures included uncorrected and corrected distance visual acuity (UDVA and CDVA, respectively), changes in higher order aberrations, low-contrast visual acuity (LCVA), binocular contrast sensitivity, and patient-reported outcome measures evaluated by validated questionnaires. Fourteen patients were also evaluated for changes in marksmanship performance using a standardized grading system.
Summary of results
Participants in this study were predominantly male (58 of 74 eyes) with a low to moderate amount of myopia and astigmatism (mean manifest sphere: –3.00 SD 1.58; mean manifest cylinder: –0.43 SD 0.39; mean manifest spherical equivalent: –3.22 SD 1.59). Most cases were performed by a single surgeon (64 of 74 eyes); 93.2% (69/74) of all cases were uncomplicated. Intraoperative complications included two eyes with cap tears, one eye with a partial cap tear involving the central axis, and two eyes with difficult dissection.
Ninety-six percent of eyes achieved an UDVA of 20/20 or better at the 3-month postoperative evaluation. The efficacy index measured as the ratio of mean postoperative UDVA to mean preoperative CDVA was 0.96. The safety index measured as the ratio of mean postoperative CDVA to mean preoperative CDVA was 1.03. There was a statistically significant increase in total higher order aberrations in addition to significant increases in coma, trefoil, and spherical aberration. LCVA was decreased in photopic (mean difference 0.03; 95% CI: 0.01, 0.06), night vision (mean difference 0.03; 95% CI: 0.00, 0.05), and mesopic conditions (mean difference 0.04; 95% CI: 0.02, 0.06) 1 month postoperatively when compared to the preoperative baseline. On average, LCVA improved at all contrast levels and conditions 3 months postoperatively (photopic [mean difference –0.01; 95% CI: –0.04, 0.02], night vision [mean difference –0.02; 95% CI: –0.04, 0.00], and mesopic [mean difference –0.01; 95% CI: –0.03, 0.01]). Eighteen of 35 patients (51.4%) were noted to have clinically significant loss of contrast sensitivity at 1 month postoperatively defined as a change of greater than or equal to 0.30 log units from the preoperative baseline at two or more spatial frequencies. Loss of contrast sensitivity was seen in seven (20.0%) of 35 patients 3 months postoperatively. A clinically significant gain of contrast sensitivity was reported in 16 of 35 patients (47.1%) at 1 and 3 months postoperatively. At the 3-month postoperative evaluation, significant improvements in patient-reported double images and starburst were reported, but there were no changes in patient-reported glare or halo. Twenty-nine of 35 patients (82.9%) reported a higher level of satisfaction with current vision at 3 months, and the overall satisfaction rating with the procedure was high at 90.9 (95% CI, 85.3, 96.5). As measured by Work Productivity and Activity Impairment scores and National Eye Institute Refractive Error Quality of Life activity limitation scores, post-SMILE procedure work limitations were limited to immediate postoperative care, and no patients reported activity impairment at 3 months. There was no statistically significant difference in marksmanship performance reported postoperatively without correction when compared to preoperative testing with correction.
The authors of this study sought to perform a similar evaluation of SMILE to provide data on a refractive surgical technique that could lead to faster visual recovery and faster return to duty.
Discussion
Many prior studies have examined corneal refractive procedures including LASIK and PRK in the context of the unique occupational demands of a U.S. military service member. The authors of this study sought to perform a similar evaluation of SMILE to provide data on a refractive surgical technique that could lead to faster visual recovery and faster return to duty.
This study suggests that based on early postoperative visual outcomes, SMILE is safe, effective, and highly predictable with a high level of patient satisfaction. The authors reported a low number of complications including difficult lenticule dissection and cap tears, which improved with increased surgical experience and standardization of surgical techniques. Low contrast visual acuity and contrast sensitivity appeared to fluctuate in the early postoperative period, though the clinical significance is uncertain given the small but statistically significant results. These findings appeared transient and normalized or improved between the 1- and 3-month postoperative evaluations. Patient satisfaction with SMILE was very high in this study, and patients noted significant improvements in double images and starbursts, but no improvements in halos or glare.
A major strength of this study is that authors assessed rifle marksmanship as an outcome measure in a subset of the study population. Six to 8 weeks following SMILE, marksmanship without optical correction slightly exceeded preoperative baseline testing with optical correction, though this difference did not achieve statistical significance.
Limitations of this study include that this was a single-center observational study with a unique study population that may limit generalizability of the study results. The study was also limited to a brief 3-month follow-up period, and refinement in the surgical technique over time may have led to outcome variability and bias. Despite these limitations, the scope of this study gives vital information to U.S. military providers in determining return to service timelines following SMILE.
During the ASCRS Journal Club, panelists discussed their personal experiences with SMILE and noted improvements in safety and efficacy of the procedure with refinements of femtosecond laser parameters and increased surgeon experience.
Small incision lenticule extraction (SMILE) in the U.S. military: prospective study of visual and military task performance
Rose Sia, MD, Denise Ryan, MS, Hind Beydoun, PhD, Jennifer Eaddy, OD, Lorie Logan, OD, Samantha Rodgers, MD, Bruce Rivers, MD
J Cataract Refract Surg. 2021;47(12):1503–1510
- Purpose: To assess early visual outcomes and military task performance following small incision lenticule extraction (SMILE) among U.S. military service members
- Setting: Warfighter Refractive Eye Surgery Program and Research Center and Night Vision and Electronic Sensors Directorate, Fort Belvoir, VA, U.S.
- Design: Single-center, prospective, observational study
- Methods: The study was comprised of active duty service members (n=37) electing to undergo SMILE for myopia or myopic astigmatism. Testing performed preoperatively and at 1 and 3 months postoperatively included uncorrected and corrected distance visual acuity (UDVA and CDVA), wavefront aberrometry, low contrast visual acuity (LCVA), contrast sensitivity, and vision-related questionnaire. Fourteen subjects underwent rifle marksmanship with spectacle correction before and without correction at 6 to 8 weeks after surgery.
- Results: At 3 months postoperatively, the efficacy index was 0.96, and the safety index was 1.03. UDVA was ≥20/20 in 96% of eyes. LCVA change from baseline was significant under night vision conditions. Eye problems contributed to 10% work and 20% activity impairments, both of which decreased to 0% (p=0.001). The overall satisfaction rating for SMILE was high at 90.9 (95% CI, 85.3–96.5), and 95% of participants would be willing to undergo the procedure again. The median scores between pre- and 6–8 weeks postoperative firing performance were comparable (34 vs. 35, with and without correction, respectively; p=0.247).
- Conclusion: After the early recovery period, SMILE seems to preserve quality of vision, which appears to facilitate the accomplishment of tasks related to their work as military service members as well as performing activities outside of work.
References
- Ito M, et al. Picosecond laser in situ keratomileusis with a 1053-nm Nd:YLF laser. J Refract Surg. 1996;12:721–728.
- Sekundo W, et al. First efficacy and safety study of femtosecond lenticule extraction for the correction of myopia: six-month results. J Cataract Refract Surg. 2008;34:1513–1520.
- Shah R, et al. Results of small incision lenticule extraction: All-in-one femtosecond laser refractive surgery. J Cataract Refract Surg. 2011;37:127–137.
- Sekundo W, et al. Small incision corneal refractive surgery using the small incision lenticule extraction (SMILE) procedure for the correction of myopia and myopic astigmatism: results of a 6 month prospective study. Br J Ophthalmol. 2011;95:335–339.
- Hjortdal JO, et al. Predictors for the outcome of small-incision lenticule extraction for myopia. J Refract Surg. 2012;28:865–871.
- FDA approves VisuMax Femtosecond Laser to surgically treat nearsightedness. FDA News Release. September 13, 2016. Accessed February 8, 2022. www.fda.gov/news-events/press-announcements/fda-approves-visumax-femtosecond-laser-surgically-treat-nearsightedness.
- Sia RK, et al. Visual outcomes after SMILE from the first-year experience at a U.S. military refractive surgery center and comparison with PRK and LASIK outcomes. J Cataract Refract Surg. 2020;46:995–1002.
Contact
Friske: tyler-friske@dmei.org
Siatkowski: RMichael-Siatkowski@dmei.org