Cornea
March 2021
by Ellen Stodola
Editorial Co-Director
When considering keratoconus, one of the most important aspects of the disease is screening and early diagnosis before being able to treat patients.
William Trattler, MD, said young patients may begin to show signs of keratoconus. Even those under age 8 may show signs on topography, he said, noting that he’s observed topographic signs in patients as young as 5 years old. There’s no hard rule as to when a screening topography should be performed, Dr. Trattler said, so the decision to perform topography is based on the eyecare provider’s suspicion that keratoconus may be present.
Dr. Trattler said you might want to consider performing a screening topography in anyone developing changes in his or her prescription. If you wait for patients to experience vision loss or show signs on the slit lamp exam, they likely will have advanced keratoconus at that point.
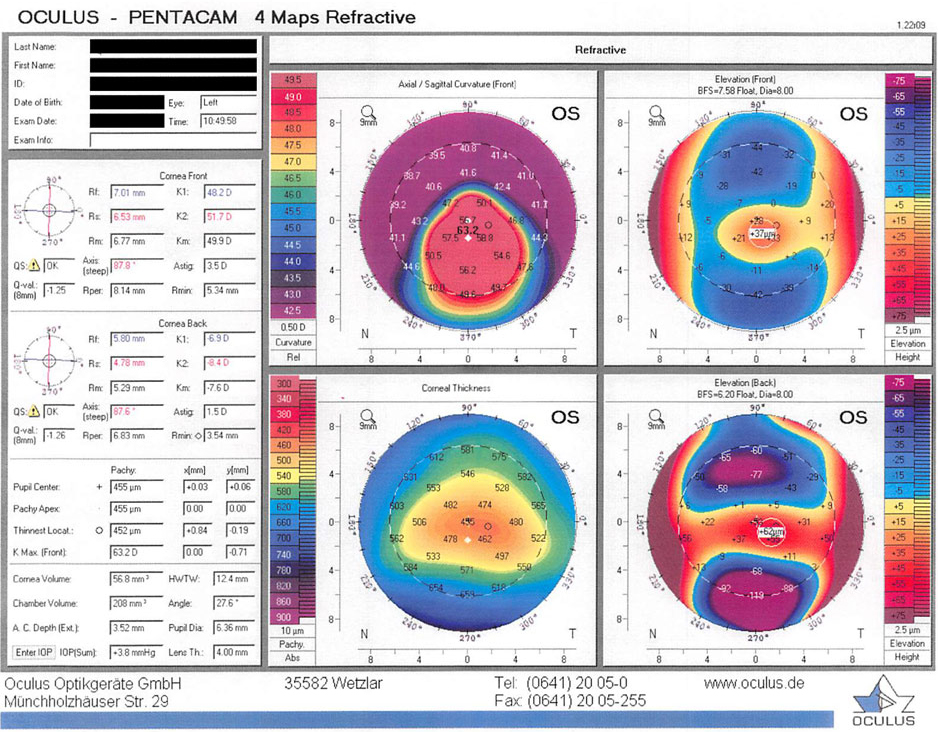
Dr. Trattler evaluates the corneal shape with topography and tomography. Topography, which images the front surface of the cornea, is effective at identifying keratoconus. Tomography evaluates both the front and back surfaces of the cornea and in some cases may identify keratoconus earlier, he added.
Dr. Trattler recommended an annual screening for patients with borderline findings of keratoconus on topography to keep tabs on whether they have any signs of keratoconus and/or if they are progressing.
Crosslinking is effective at stopping the progression of keratoconus, which if caught and treated early enough can prevent significant vision loss. Crosslinking is currently FDA approved for ages 14 and older, but Dr. Trattler said he has treated some younger patients with keratoconus.
He said he thinks keratoconus screening as a whole could be significantly improved, as many patients get diagnosed with moderate to severe disease. Patients interested in refractive surgery including LASIK undergo topography screening, and a surprising number of patients with keratoconus are identified. If patients returning for their annual checkups for contact lenses were screened, it’s likely many patients would be identified with keratoconus and at an earlier stage than is happening now. “Studies looking at the incidence and prevalence of keratoconus have found a much higher percentage of patients with keratoconus than people realize,” he said.
Ken Beckman, MD, agreed that early diagnosis for these patients is key. “While the incidence has been described as 1 in 2,000, it now appears to be much higher,” he said. “The key to managing these patients is early diagnosis. Our current treatment, crosslinking, works best when we catch patients in an early stage.” He added that the current treatment protocol often waits until some vision is lost, which is missing some of the maximum benefit. However, he said that even late-stage cones can benefit from treatment.
Dr. Beckman usually recommends that grade school children undergo regular vision screenings, and if decreased vision is detected, further evaluation is warranted.
Dr. Beckman said that screening starts with visual acuity and refraction. “Patients with decreased vision, progressive myopia, or significant astigmatism are at greater risk and may merit evaluation with topography/tomography.” Other tests that can help, particularly if a topographer is not available, can be looking for scissoring on retinoscopy, along with the slit lamp exam findings. He likes to image both the front and back of the cornea to have as much information as possible using the Pentacam (Oculus), which he said has excellent diagnostic images to aid in identifying cones and monitoring for progression.
If a patient is progressing and at risk for vision loss, even very young patients can be treated, he stressed. “While the label for the FDA approved Avedro device [Glaukos] indicates patients 14 and older, often patients even younger need to be treated,” he said. “If the patient is mature enough to hold still for the treatment, they may be able to undergo it as young as 10 or even younger. I have not treated anyone under 12, but I would if needed.”
About the physicians
Ken Beckman, MD
Comprehensive EyeCare of Central Ohio
Westerville, Ohio
William Trattler, MD
Center for Excellence in Eye Care
Miami, Florida
Relevant disclosures
Beckman: Glaukos
Trattler: Glaukos, CXLO, Oculus
Contact
Beckman: kenbeckman22@aol.com
Trattler: wtrattler@gmail.com