Cornea
September 2021
by Ellen Stodola
Editorial Co-Director
With neurotrophic keratitis (NK), there is a lot to consider in terms of staging, making a diagnosis, and treatment. Three experts discussed how they work up NK patients and some of the options for handling these cases.
Stages of NK
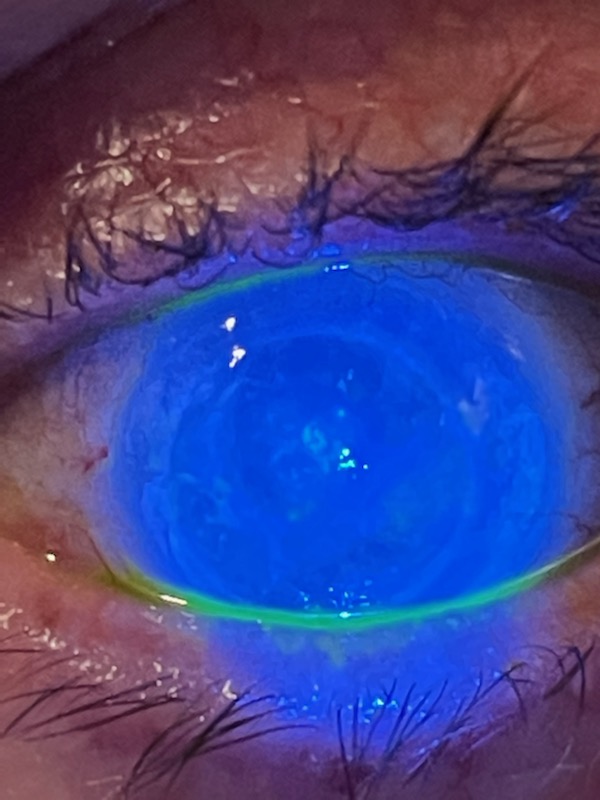
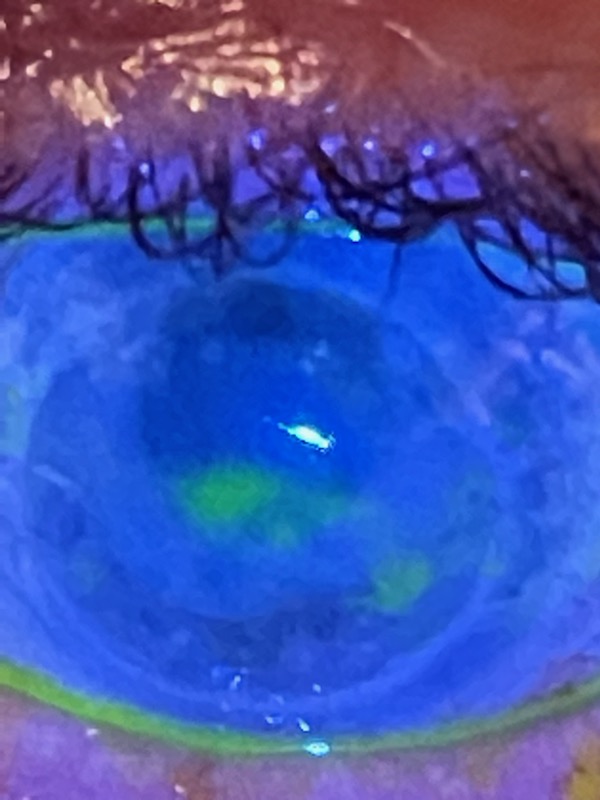
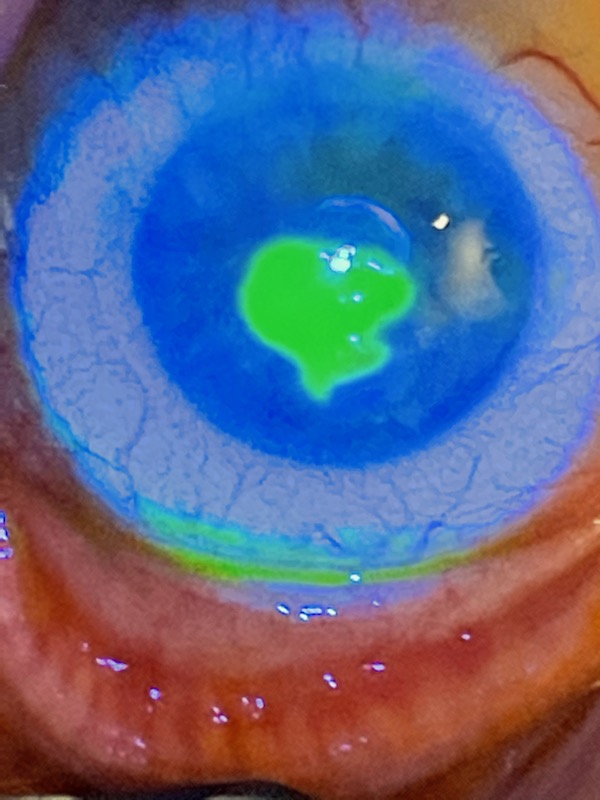
When staging NK, Kenneth Beckman, MD, said that he separates corneal sensation into normal, decreased, and absent. “Once I establish that they have decreased sensation, and if they have signs of keratitis, I usually separate into the three traditional categories: Stage 1 is punctate epithelial changes but no true defect. Stage 2 is a defect but no thinning. Stage 3 is a defect with thinning,” he said. “I don’t use the stage number per se, but I describe the cornea based on those criteria.”
“Unfortunately, people don’t think about NK until it’s a round corneal ulcer and scarring, and that’s when the light bulb goes off.”
Edward Holland, MD
Edward Holland, MD, was involved in a neurotrophic keratitis study group that worked on an updated staging criteria for NK. “We put together a white paper that’s been submitted for publication,” he said. Dr. Beckman was part of this group as well, along with Albert Cheung, MD, Marjan Farid, MD, Nicole Fram, MD, Preeya Gupta, MD, W. Barry Lee, MD, Francis Mah, MD, Mark Mannis, MD, Jay Pepose, MD, and Elmer Tu, MD.
The Mackie classification has been used for staging NK. It starts with Stage 1, which is staining of the inferior conjunctiva and decreased TBUT and punctate staining of the cornea. Stage 2 is epithelial defect with stromal folds and swelling, and Stage 3 is corneal ulcer and melting, Dr. Holland said. “We thought this didn’t represent all the various stages,” he said.
The study group proposed the following classifications:
- Stage 0: Altered sensation without any keratopathy
- Stage 1: Corneal epitheliopathy without any stromal involvement
- Stage 2: Punctate epithelial keratopathy with anterior stromal haze
- Stage 3: Persistent or recurrent epithelial defects
- Stage 4: Persistent or recurrent epithelial defects with stromal scarring but no ulceration
- Stage 5: Persistent or recurrent epithelial defects with corneal ulceration
- Stage 6: Corneal perforation
“We have patients who have epitheliopathy without stromal involvement, and we have patients with epitheliopathy with stromal haze but who don’t have persistent epithelial defect,” Dr. Holland said. “Our Stage 2 is where a lot of patients get diagnosed with dry eye when we want physicians thinking about NK.”
Dr. Holland said the hope is that this will provide more understanding that there are many stages. “Unfortunately, people don’t think about NK until it’s a round corneal ulcer and scarring, and that’s when the light bulb goes off,” he said.
Clinical diagnosis of NK
When doing a workup for the clinical diagnosis of NK, Asim Ali, MD, said he’s trying to figure out the etiology. For example, if you know there’s a clear history of herpes, that makes it more straightforward, he said. If it’s completely out of the blue, you might have to do an MRI to rule out structural problems in the brain or tumors.
The workup will depend on how the patient presents and if you can distinguish between a cause that’s in the eye itself.
In making a clinical diagnosis, Dr. Holland said the number one thing is to have a differential diagnosis.
Dr. Holland also stressed that it’s not necessary to have a quantified professional aesthesiometer. “A lot of people used to use the tip of a cotton swab but even easier is the edge of tissue paper or piece of dental floss,” he said, adding that corneal sensation should be in the workup.
Dr. Beckman said that when making a clinical diagnosis it’s important to do staining to establish that the patient has keratitis in general. Then he will check sensation if they have staining or a defect and if he is suspicious of NK.
“If they have decreased sensation, I typically treat as NK,” Dr. Beckman said. “I understand that many patients may have decreased sensation and coexisting epithelial disease, but the neurotrophic cornea may not have caused the keratitis.” He added that it may be dry eye, medication toxicity, or something else. “I treat with traditional methods first, but if they have these findings and do not respond to conventional treatment, I treat as NK,” Dr. Beckman said.
Systemic diseases associated with NK and NK from herpes
Dr. Beckman has found that the two most common systemic diseases associated with NK are diabetes and MS.
NK can also be associated with herpes. Dr. Beckman said he hasn’t found a big difference between herpes simplex and herpes zoster in severity. “The one curveball is that with herpes simplex, we need to determine if there is active viral keratitis requiring antiviral therapy rather than just treatment for NK,” he said. “I prefer oral antivirals, particularly because they don’t have the toxicity that topical therapy does.”
Dr. Holland said there are a number of conditions that can be associated with NK. In addition to herpes simplex and herpes zoster, he said that any severe infection on the cornea or severe injuries, like chemical burns, can lead to NK. Other factors like LSCD and chronic contact lens wear can also be associated.
Dr. Holland added that you can see NK from ocular surgeries, such as PK or DALK, refractive corneal surgery, or any procedure that removes epithelium. Medications can also be associated with NK. Dr. Holland said there are some congenital causes as well, though these are generally rare.
Treatments
There are a number of treatments for NK that physicians can employ at various stages and depending on the individual patient.
According to Dr. Holland, it’s a “step ladder approach” based on the severity.
In the early steps, it’s important to add preservative-free lubrication and remove any toxic topical medications, which can cause dryness on the surface, Dr. Holland said. If there is ocular surface disease, it should be treated with preservative-free drops, ointments, omega-3s, etc.
Different types of contact lenses can also be used. Dr. Holland will use bandage contact lenses as aearly treatment. “If there’s confluent punctate staining and I’m worried about scarring or ulceration, I want to be aggressive with an early bandage contact lens,” he said.
Dr. Beckman also said he uses a bandage contact lens to treat a persistent defect. “Initially, for NK, I treat these patients the same as non-neurotrophic corneas with persistent defect, and bandage contact lenses are used very early,” he said. “I may add amniotic membrane to those as well.” Dr. Beckman added that the main risk with a contact lens is infection, so antibiotics are typically used. “Of course, the more drops that are used, the greater the risk of toxicity compromising healing, so it must be a balance,” he said.
A scleral contact lens may be helpful, and Dr. Beckman said these can be particularly useful in cases of non-healing defects and dry eye, though they can be expensive. “Some vision insurances will cover scleral lenses for certain diagnoses, but NK may not be covered,” he said. “If these are attainable, they can work very well.”
Dr. Ali agreed that scleral lenses can be helpful, particularly the PROSE treatment. These can work well for someone with stable NK, he said, as they help with the epithelial surface.
Autologous serum tears are another potential treatment for NK. “They provide growth factors that aid in epithelial healing,” Dr. Beckman said. There may be some challenges in access and obtaining these. Dr. Beckman works with a local lab that draws the blood and spins it down to remove the blood cells, leaving the serum to be converted into the tear formula. “It is important to establish a relationship with a local lab to do the draw and spinning,” he said. “Then a compounding pharmacy can make the formulation.”
Dr. Beckman noted that there are sterility risks since the tears are not preserved. “Typically, they are kept frozen, and a small amount can be thawed but kept refrigerated for use,” he said, adding that the compounding pharmacy will let the patient know the expiration date.
“There is a small risk for infection because it is non-preserved and made from blood products, but it is typically well tolerated,” he said. “I often tell patients that they can use the drops even 4–6 times per day as needed.”
Amniotic membrane is another treatment option. Dr. Ali said he uses this, though noted that it doesn’t work all the time.
Conjunctival grafts can be used in the treatment of NK, though Dr. Beckman said that this is not as common since Oxervate (cenegermin-bkbj, Dompe) is now available, and other treatments like amniotic membrane or tarsorrhaphy can be used. However, this option may be useful for advanced non-responsive cases.
Dr. Ali also said conjunctival grafts can be useful, but they don’t restore sight. These prevent breakdown and infections, but you’re damaging the ocular surface permanently, he said. Once you do a conjunctival graft, you can’t go back easily.
Dr. Ali likes to employ lateral tarsorrhaphy when possible because he said it’s very effective. “Patients generally don’t want them for obvious cosmetic reasons,” he said.
“I think this is one of the most underused procedures we have to manage corneal disease, especially in NK,” Dr. Holland said.
Dr. Holland said whether tarsorrhaphy is used often depends on the patient’s age and whether or not it’s socially acceptable. A young patient who is active doesn’t want a 70% tarsorrhaphy, he said, but if you have an elderly patient with poor visual potential in this eye who isn’t driving and isn’t very active, it could be a good option, particularly if it’s a patient who has to see the eyecare provider frequently for a persistent epithelial defect.
It can help get the patient stable, prevent progression, heal the defect, and reduce their dependence on someone taking them to appointments, he added. “Every tarsorrhaphy can be reversed, but it’s a bit more difficult to get buy-in from younger patients,” Dr. Holland said.
Dr. Beckman said he prefers a traditional sutured tarsorrhaphy as it may need to remain for an indefinite period because the underlying cause of NK may continue indefinitely.
Oxervate
Oxervate is the first medication approved for treatment of NK. It is a recombinant form of human nerve growth factor that helps regenerate nerve function in the cornea and restore the health of the corneal surface, Dr. Beckman said. “It is covered by insurance, but often requires going through some hoops to get it approved,” he said. “In my experience, it works very well. I have treated numerous patients with Oxervate and have been impressed.”
Dr. Holland said he has had good experience so far using Oxervate. It works in some patients extremely well and in others not as well, he said. “I see it work well when the NK is not extremely longstanding and the patients are a bit younger.” Severe NK in older patients doesn’t tend to respond as well, he said.
Corneal neurotization
Corneal neurotization is a newer treatment approach. Both Dr. Beckman and Dr. Holland said they are not currently performing this procedure. Dr. Beckman noted that he works with another specialist who is performing the procedure and said it seems promising.
Dr. Ali was involved in pioneering this approach. He’s had about 6 years of experience, having been involved in publications1,2 that described the technique. He uses nerve grafts but noted that allografts and nerve transfers can also be used in this process.
Corneal neurotization, he said, uses nerve grafts to connect nerves intact on the face to the eye or both eyes with neurotrophic disease. The nerves then grow down the grafts and into the cornea. He noted that this would not be a first-line treatment.
The procedure can’t be compared easily to other treatments because of how it works and how it fits in the treatment paradigm, he said. Oxervate would be the closest treatment, but there are no head-to-head comparisons, and Oxervate works differently, particularly in terms of healing the epithelium but not as much in improving sensation. Studies on neurotization have focused more on restoration of sensation. Neurotization takes a lot longer to be effective and works in a different way, he said.
Corneal neurotization is more involved because of the amount of surgery needed. He said there are a number of techniques/modifications that are being used successfully as well.
About the physicians
Asim Ali, MD
Professor of Ophthalmology & Vision Sciences
University of Toronto
The Hospital for Sick Children
Toronto, Canada
Kenneth Beckman, MD
Clinical Assistant Professor of Ophthalmology
Ohio State University
Columbus, Ohio
Edward Holland, MD
Professor of Ophthalmology
University of Cincinnati
Cincinnati, Ohio
References
- Elbaz U, et al. Restoration of corneal sensation with regional nerve transfers and nerve grafts: a new approach to a difficult problem. JAMA Ophthalmol. 2014;132:1289–1295.
- Bains RD, et al. Corneal neurotization from the supratrochlear nerve with sural nerve grafts: a minimally invasive approach. Plast Reconstr Surg. 2015;135:397e–400e.
Relevant disclosures
Ali: None
Beckman: Dompe
Holland: Dompe
Contact
Ali: asim.ali@utoronto.ca
Beckman: kenbeckman22@aol.com
Holland: eholland@holprovision.com