Ophthalmology News
February 2008
by Vanessa Caceres
EyeWorld Contributing Editor
… but they’re not without their risks

As allergies increase worldwide and as ocular allergies garner greater attention, more of your patients may use oral medications or intranasal steroids in addition to topical eye drops for allergic rhinoconjunctivitis. However, it would be prudent to monitor who among your patients is prescribed these allergy treatments. As a minor irritation, they may cause dryness. More seriously, these treatments may occasionally lead to cataracts in certain patients or a rise in IOP in glaucoma patients.
A report in a recent issue of Allergy and Asthma Proceedings cited a survey that found 14.2% of the adult U.S. population has been diagnosed with allergic rhinoconjunctivitis. According to some epidemiologic studies, conjunctivitis symptoms are at least as severe as rhinitis symptoms in approximately 70% of patients with hay fever as seen in the 1998 issue of Schweizerische medizinische Wochenschrift, said John K. Lawson, M.D., Rush University Medical Center, Allergy/Immunology, Chicago. As patients don’t typically want to start their allergy treatments taking multiple medicines, Dr. Lawson noted it is common to begin treatment with antihistamines or intranasal steroids. “Sometimes that’s all they need. If they don’t respond to that, I’ll add a topical ocular antihistamine,” he said.
Still, Dr. Lawson and ophthalmologists are finding good reasons to proceed with some caution when treating allergies with oral medications or nasal steroids, due to possible side effects.
Antihistamines: the drying effect
Older antihistamines often dried out patients’ eyes, either causing general dryness not present before or exacerbating an existing dry-eye condition, said Esen K. Akpek, M.D., associate professor of ophthalmology and director, Ocular Surface Diseases and Dry Eye Clinic, Wilmer Eye Institute, Johns Hopkins University, Baltimore.
The newer antihistamines don’t have as much of a drying effect; still, some patients still notice more dryness, said Leonard Bielory, M.D., professor of medicine, pediatrics, and ophthalmology and visual sciences, and director, Division of Allergy, Immunology and Rheumatology, University of Medicine and Dentistry of New Jersey, New Jersey Medical School, Newark. This is especially common in female patients over the age of 40. “Although [the medications] may tremendously help nasal symptoms, their eyes can become excessively dry … The newer ones have less of an effect, but they’re not zero,” Dr. Bielory said. Some studies report a more marked effect with certain antihistamines compared with other forms of treatment. For example, a 2004 study published in the Annals of Allergy Asthma and Immunology found that Clartin (loratadine, Schering-Plough, Kenilworth, N.J.) induced significantly more conjunctival staining than Zyrtec (cetirizine hydrochloride, Pfizer, New York). However, both drugs “induced signs and symptoms associated with ocular dryness, including increased corneal and conjunctival staining, decreased tear film break-up time, and increased ocular discomfort in healthy individuals,” the investigators wrote.
Another study, published in the April 2007 issue of Clinical Therapeutics, compared once-daily dosing of loratadine 10 mg and Elestat (epinastine hydrochloride ophthalmic solution, Inspire Pharmaceuticals/Allergan, Irvine, Calif.) in patients with seasonal allergic conjunctivitis. That research found loratadine was associated with a 33.7% reduction in tear volume, a 35% reduction in tear flow, and a 21.7% increase in global fluorescein staining.
Reported problems with certain antihistamines such as these steer more clinicians toward topical medications, such as eye drops.
“In a recent report, more than 80% of patients taking oral antihistamines for their allergic ‘rhinoconjunctivitis’ still had ocular allergy symptoms,” Dr. Bielory wrote in a 2006 issue of Current Allergy and Asthma Reports. “The lack of effect of oral agents in ocular allergies suggests that one should consider a more topical approach to treat ocular allergy to improve the quality of life of patients suffering from allergic ‘conjunctivo-rhinitis’.”
Depending on the extent of the dryness, Dr. Lawson will recommend that patients use artificial tears. This helps alleviate the ocular irritation caused by the dryness and may also help eliminate allergens from the eye, he said.
Dr. Bielory also leans more toward the use of nasal steroids or topical agents in these patients if ocular allergies are their primary concern. “Nasal steroids appear to have a class effect on ocular symptoms,” he said.
Nasal steroids and IOP
As Dr. Bielory said, intranasal steroids appear to help both allergic rhinitis and allergic conjunctivitis.
A new nasal spray that has advertised heavily to consumers, Veramys nasal spray (fluticasone furoate, GlaxoSmithKline, Middlesex, United Kingdom), even touts in its advertising its dual effect on nasal and ocular allergy symptoms.
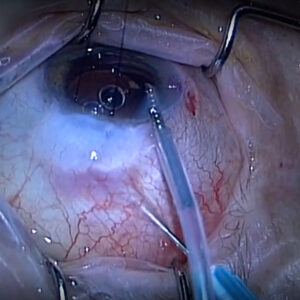
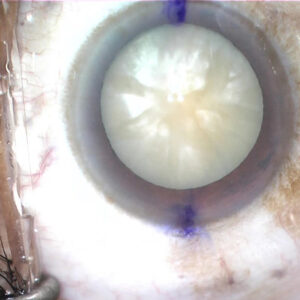
However, many times, patients have not been told by their allergy doctor that they are using a steroid. Use of steroids can lead to cataracts in some patients or IOP rises in glaucoma patients.
“When we ask about their medications, they don’t consider a nose spray to be a medication. They think of it like a vitamin,” said Karen M. Joos, M.D., Ph.D., associate professor of ophthalmology and visual sciences, Vanderbilt University Medical Center, Nashville.
As an example, “I had a glaucoma patient whose pressure had gone up, and he wasn’t sure why,” Dr. Joos said. When she asked about other medications he was taking, he referred to a “nose spray.” Unbeknowst to him, it was a steroid nose spray. When he stopped using it, his pressure went down.
This led Dr. Joos and co-investigators to research the effects of intranasal steroids in 12 glaucoma patients. They found a significant reduction in IOP with nasal steroid discontinuation in these patients. The mean IOP for each pair of eyes was 15.4 mm Hg before they were taking steroids, 18 mm Hg during the steroid use examination, 14.5 mm Hg for the first post-steroid use examination, and 14.8 mm Hg for the second post-steroid use examination.
Eleven of the 12 patients experienced a decreased average IOP at the first post-steroid use exam, which usually took place 35 days after they stopped nasal spray use.
This was published in a 2005 issue of The Journal of Allergy and Clinical Immunology.
Although the study has its limitations, Dr. Joos said it still seems to indicate that “steroid nose sprays may contribute to elevated pressure just like every other steroid modality that we use.”
“All steroids, in the form of drops or an injection, can raise pressure,” said Alan L. Robin, M.D., associate professor of ophthalmology and associate professor of international health, Bloomberg School of Public Health, Johns Hopkins University, Baltimore. The IOP may only rise 1 or 2 mm Hg, but the actual effect often depends on the frequency and amount with which glaucoma patients use that particular medication.
Cataracts are another occasional side effect from patients that use steroids, but they more often form in patients who have used steroids for a long time, Dr. Akpek said.
The patients with an increased risk are those with a family history of glaucoma or with other risk factors for cataract, such as smoking and diabetes mellitus, Dr. Lawson said.
“Our general recommendation is that these patients be vigilant about their eye exam,” he said. If an allergy patient has a family history of glaucoma or cataract, he still will often prescribe nasal steroids but urge the patient to have regular eye exams. If the patient already has cataract or glaucoma and requires allergy medications, he will try other classes of drugs including leukotriene receptor antagonists, such as Singulair (montelukast sodium, Merck, Whitehouse Station, N.J.), or topical and systemic antihistamines. Clinicians prescribing nasal steroids should make it clear to patients what they are prescribing and its possible side effects, Dr. Joos and co-investigators wrote in their study. “Providers should consider inquiring about a history of glaucoma before prescribing a steroid intervention and consider alternative therapy for patients given a diagnosis of glaucoma or recommend monitoring the IOP by the patient’s ophthalmologist,” they wrote.
Ophthalmologists should also make a point to ask glaucoma patients about their specific use of nasal sprays as well as steroids, the study concluded.
ARTICLE SIDEBAR
Monitor allergy meds’ effects in your patients
Talking points with your allergy patients
- Are you taking antihistamines for your allergies?
- Are you experiencing increased dry eye?
- Do you have a family history of glaucoma and/or cataract?
Talking points with your glaucoma patients who have allergies
- In addition to your regular medications, are you using any nasal sprays? (You can then inquire about the type of nose spray to see if it is an intranasal steroid and if additional IOP monitory is required.)
Ocular-related talking points for allergists and their patients
- Do you experience dry eye? (Watch out for the drying effect of antihistamines)
- Do you have glaucoma? (Nasal steroids may increase glaucoma patients’ IOP.)
- Do you have a family history of glaucoma and/or cataract?
Editors’ note
Dr. Akpek has financial interests with Inspire Pharmaceuticals (Durham, N.C.). Dr. Bielory has financial interests with Genentech (South San Francisco, Calif.), Novartis (Basel, Switzerland), Pfizer (New York), and Santen (Napa, Calif.), among others. Dr. Robin has financial interests with Alcon (Fort Worth, Texas), Ista Pharmaceuticals (Irvine, Calif.), and Merck (Whitehouse Station, N.J.). Drs. Joos and Lawson have no financial interests related to their comments.
Contact Information
Akpek: 410-955-5494, esakpek@jhmi.edu
Bielory: 973-972-2768, bielory@umdnj.edu
Joos: Karen.joos@vanderbilt.edu
Lawson: 312-942-4914, John_Lawson@rush.edu
Robin: 410-377-2422, glaucomaexpert@cs.com