Refractive Surgery: Device focus
June 2014
by Michelle Dalton
EyeWorld Contributing Writer
For some surgeons, these lenses offer hope to high myopes. For others, the potential complications outweigh the potential benefits
Editors’ note: This column discusses technologies that are not commercially available in the U.S.
The correction of high myopia is limited, but phakic IOLs do provide a surgical option. “For many years we have been looking for a quality anterior chamber phakic IOL that could be easily performed in a clean room rather than an operating room,” said Eric D. Donnenfeld, MD, partner at Ophthalmic Consultants of Long Island, Rockville Centre, N.Y., and clinical professor of ophthalmology, New York University Medical School.
With only two phakic lenses available in the U.S.—the Verisyse (Abbott Medical Optics, Santa Ana, Calif.) and the Visian (STAAR Surgical, Monrovia, Calif.)—options for U.S. physicians will remain limited.
A third lens, the Cachet (Alcon, Fort Worth, Texas), remains in clinical studies, as does a foldable version of the Verisyse (Veriflex, Abbott Medical Optics); the Visian ICL with CentraFlow (STAAR Surgical) is not available in the U.S.
Neither the Verisyse nor the ICL is a perfect solution, said Kerry K. Assil, MD, medical director and chief executive officer, Assil Eye Institute, Beverly Hills and Santa Monica, Calif.
“People have looked for a better mousetrap but haven’t been able to come up with one yet,” he said. Alternative attempts have focused on developing angle-fixated, anterior chamber IOLs, which have generally failed, as these lenses sit too close to the peripheral endothelium and also caused “unacceptable iris root inflammation. That chronic low grade trauma may eventually lead to the ovalization of the pupil,” among other issues, Dr. Assil said.
Richard L. Lindstrom, MD, founder, Minnesota Eye Consultants, Minneapolis, said those kinds of complications are why he stopped implanting phakic lenses 2 years ago.
“I was quite excited about the Alcon Cachet, but it is now showing select cases of late PAS, pupil ovaling, and unpredictable endothelial cell loss. I am also seeing late cases of cataract, pigment dispersion, secondary glaucoma, and unexpected endothelial cell loss with the Visian,” he said. His best long-term results have been with the Verisyse, “but I have seen erosion through the iris and subluxations here in select cases as well, and patients often are unaware of their problem.”
As most surgeons can confirm, phakic IOL patients are also more likely to develop cataract/dysfunctional lens syndrome in their 50s. Additionally, the majority “has significant astigmatism. And they’re young, so you shouldn’t preform relaxing incisions,” said Jeffrey D. Horn, MD, in private practice, Vision for Life, Nashville, Tenn. “Ideally, we’d like to go in with a lens that could correct the refraction and astigmatism in one fell swoop.”
While the field has been stagnant for a while, the FDA recently approved the Visian toric, “which should be a significant addition to our armamentarium,” Dr. Donnenfeld said.
Below, an update on current phakic IOLs.
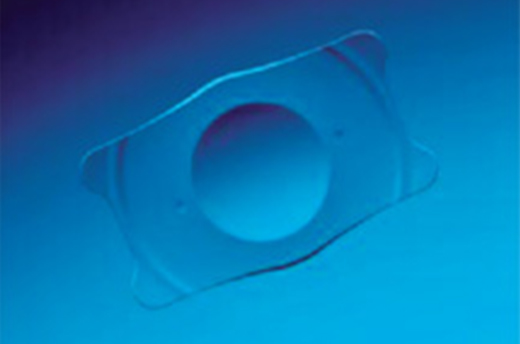
Cachet
Dr. Horn, a principal investigator for the Cachet since its phase 2 studies, said that in his hands, complications have been few. He’s implanted 53 patients.
“I did have to reposition the lens in a couple of patients, but that’s not unique,” he said. Some patients do experience a greater cell loss than anticipated, however. “It’s why I think the lens is on the back burner,” he said, although there is an active 10-year study. In the one patient with a “cell count that was lower and dropping faster than we would like,” Dr. Horn said he explanted the Cachet. “The lens was vaulting closer to the corneal endothelium than almost all of the other patients that I had.” Yet these patients remain some of his happiest, he said.
The Cachet “has been shown to be better than previous generation anterior chamber phakic IOLs; it is demonstrating the same complications of previous generation lenses but with a reduced incidence,” Dr. Donnenfeld said.
During the implantation phase of the studies, Dr. Horn noted that the lens did have some rotation that did not alter visual outcomes, but would make it an unlikely platform for a toric version, should the lens be submitted for U.S. regulatory approval.
Verisyse/Artisan
In addition to serving high myopes, in the “right type of keratoconic patient,” the Verisyse lens “does extremely well over time,” Dr. Assil said. “These lenses have helped to avoid the alternative option of corneal transplantation on multiple occasions. Outside the U.S., this is the most popular lens in the world as a secondary IOL (in remedying aphakia).”
There are two versions of the Verisyse, one of which is foldable, Dr. Assil said. The foldable version is not available in the U.S.
“What I like about this lens is that it doesn’t cause cataracts because it sits in the anterior chamber and also relatively far from the endothelium,” he said. “In a very tiny subset, it can create endothelial cell loss over time, necessitating explantation (in less than 1% of implanted patients).” That subset includes those with shallow chambers or vigorous eye rubbers—people who should be excluded from receiving the lens in the first place, which comprises a small percentage of the potential patient population, he said.
Because a foldable version is not available in the U.S., this lens “requires slightly greater surgeon skill to reliably implant,” Dr. Assil said. “However, having implanted the Verisyse for 18 years, I have encountered surprisingly few issues with either the initial astigmatism management or long-term drift. This has also been the experience of the industry with more than 40 years of use.”
“The non-foldable version requires a 6 mm entry wound. Manipulation of that entry wound is more demanding than the remainder of the lens implantation.” Dr. Horn said the large incision size also makes it more difficult to control astigmatism.
“It just strikes me as the wrong way to do a refractive surgical procedure when the goal should be to minimize the incision size and lessen the chance of induced astigmatism,” he said, adding potential complications such as high pressures and permanently fixed, dilated pupils have dissuaded him from using the lens.
“No lens is perfect, but the idea you’re going to have to clip this lens onto the iris with a human lens behind it when you know you can put an ICL right behind the eye makes little sense to me,” he said.
Dr. Donnenfeld said he used the Verisyse “for many years,” but in his hands required peribulbar anesthesia, a larger wound, and the need for sutures. However, late complications (dislocation and cataract formation) are rare, “and this lens has a 20-year track record.”
Visian ICL
This lens is “very easy” to insert, Dr. Horn said, but did acknowledge cataract formation is higher in patients with the ICL.
The newer iterations have “reduced the propensity for cataract formation” as different sizes fit into the sulcus better, Dr. Assil said. “By introducing the pinhole opening in the center of the lens, some believe that it may also improve aqueous dynamics and diminish cataract formation over time, although that’s not so clear at this time.” The Visian ICL with CentraFlow lens is not available in the U.S.
The ongoing challenge with this lens platform, Dr. Assil said, is that it sits behind the iris and “comes into intimate contact with the anterior lens capsule, and in some patients, by being adjacent to the iris pigment epithelium, it can cause mild pigment dispersion, prolonged inflammation, and pigmentary glaucoma.”
Yet, if the CentraFlow was available, Dr. Assil “would love to use it on a subset of patients.”
Dr. Horn has explanted about 10 ICLs because of cataract formation, although he did not implant the lenses; “cataract formation is higher than we initially thought and it’s higher than in the FDA studies,” he said.
Given the choice, however, Dr. Horn would still prefer to implant the Cachet.
In an ideal world
Dr. Donnenfeld puts the Visian with CentraFlow on his wish list, as “it has no visual side effects and eliminates the need for two iridotomies that we now perform with all of our ICL cases. In addition I would like to see the Verisyse lens in the United States in a hyperopic version available as a secondary IOL for aphakia. This lens would offer significant advantages over current generation anterior chamber IOLs in many cases.”
For the time being, Dr. Assil will continue to use both available lenses (while preferring the Verisyse), but holds out hope that the U.S. will approve other phakic lenses.
Ideally, he would like to use the Veriflex, with the Visian with CentraFlow as his second choice. “While none of these lenses can be implanted without periodic surveillance, it is important to remember that these lenses are far safer than either LASIK or refractive lens exchange (RLE) in this patient population. To steer the field away altogether would irresponsibly promote overutilization of these alternative approaches along with their associated complications of corneal ectasia (LASIK) and retinal detachment (RLE),” Dr. Assil said. “As long as the Cachet is unapproved, I prefer the Visian to the Verisyse,” Dr. Horn said. “Ideally, I’d like to see the Cachet commercially available. It would definitely be my lens of choice.”
Editors’ note
Dr. Assil has financial interests with Abbott Medical Optics. Dr. Horn is a principal investigator for the Cachet lens. Drs. Donnenfeld and Lindstrom have financial interests with Abbott Medical Optics and Alcon.
Contact information
Assil: info@assileye.com
Donnenfeld: ericdonnenfeld@gmail.com
Horn: Jeff.Horn@bestvisionforlife.com
Lindstrom: rllindstrom@mneye.com