Cornea
April 2023
by Liz Hillman
Editorial Co-Director
Amniotic membrane, in its various forms, has several ophthalmic applications, but it is also, at times, being marketed for indications that don’t have a lot of evidence in the scientific literature and/or that have other proven alternatives, according to physicians.
Kourtney Houser, MD, said there are a number of companies that offer dehydrated and cryopreserved amniotic membrane. John Hovanesian, MD, said amniotic cytokine extract drops are also being produced.
Overall, amniotic products are sought after for their anti-fibrotic and anti-inflammatory properties that facilitate healing. Just when use of these products makes sense, however, is up for debate.
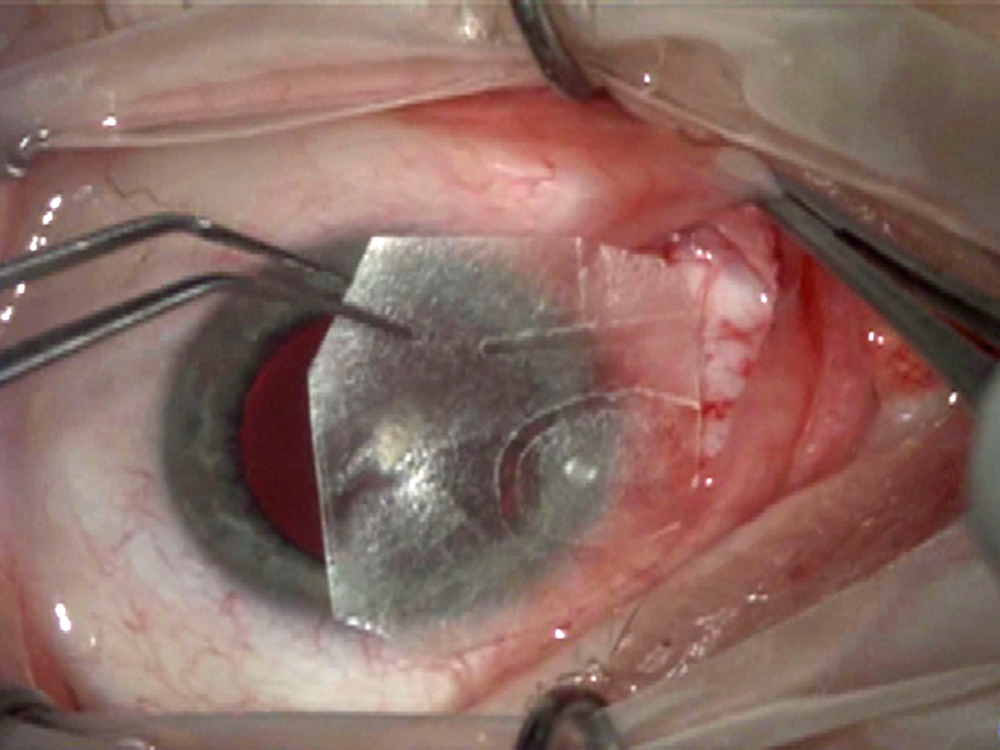
Source: John Hovanesian, MD
Dr. Houser said there are several scenarios when she will consider using amniotic membrane, such as in cases of persistent epithelial defect occurring spontaneously or following procedures such as superficial keratectomy, PTK, PRK, band chelation, or crosslinking. Patients with etiologies that are at high risk for prolonged healing following epithelial removal, such as autoimmune disorders, underlying severe dry eye, or neurotrophic keratopathy, can benefit from application of amniotic membrane concurrent with one of the above procedures, she said.
“I will occasionally use amniotic membrane in high-risk patients in conjunction with superficial keratectomy. If the epithelium is not healing appropriately and nearly completely healed at 1 week following a procedure involving epithelial removal such as superficial keratectomy or PTK, I will often place an amniotic membrane to facilitate healing,” Dr. Houser said. “I also find amniotic membrane to be helpful in patients with neurotrophic ulcers and often will use it in conjunction with other treatment modalities such as serum tears or a tarsorrhaphy or while awaiting approval and receipt of cenegermin.”
“Especially in cases where we would like to heal the ocular surface quickly, such as patients having a flare from their baseline dry eye or patients in whom we are trying to optimize the ocular surface prior to cataract surgery and who can’t tolerate steroid drops, amniotic membrane can be a useful adjuvant treatment to other longer-term maintenance therapies.”
Kourtney Houser, MD
Dr. Hovanesian also mentioned the use of amniotic membrane for persistent ocular surface defects but said that it’s important to address underlying causes of those defects. For example, if a patient has an eyelid defect that is causing the surface issue, the issue will persist if the eyelid problem is not solved.
“You have to address the underlying issues,” Dr. Hovanesian said. “Amniotic membrane may still be appropriate in these cases, but you’ve done the patient little good if the surface breaks down 2 weeks later because the eyelid is not closing.”
Dr. Hovanesian and Dr. Houser said they sometimes use amniotic membrane after pterygium excision as well. While both use conjunctival autografts, Dr. Hovanesian said research has found that putting an amniotic membrane in the subconjunctival space around the autograft, though not under the graft, promotes healing.
“It serves in that location as a biologic depot, using its anti-inflammatory and anti-fibrotic properties to reduce the growth of fibrotic cells that would cause recurrence, similar to the effect of mitomycin-C but without the risk,” Dr. Hovanesian said, noting that studies have found reoccurrence of pterygia after autograft alone vs. autograft plus amnion is 3–5% vs. 1%, respectively.
“I regularly use amniotic membrane for double pterygium excisions or in patients with limited conjunctiva available for an autograft who are undergoing pterygium excision, high-risk corneal transplants, keratolimbal autografts, persistent epithelial defects after corneal ulcer resolution, and in a multi-layered fashion in microperforations in patients at high risk for patching or transplantation,” Dr. Houser said, adding another cause where she’d use amnion. “Glued and sutured amniotic membrane with a symblepharon ring in patients with active Stevens-Johnson syndrome or following chemical burns is also key in preventing long-term irreversible damage to the ocular surface.”
Where use of amniotic membrane might be overkill, Dr. Hovanesian said, is in many cases of dry eye. He said that optometric colleagues often ask him about it, telling him that they’re hearing promotion about its use for dry eye patients.
“Some of the reps seem to be over representing the utility of amniotic membrane for routine dry eye,” Dr. Hovanesian said, noting that “financially there is a strong incentive for reps to sell amnion and for doctors to use it, but that’s not what we’re here for.”
There is promising anecdotal evidence for liquid amniotic cytokine drops, for example, but Dr. Hovanesian said that physicians prefer more rigorous science to support the use of these products.
“There are cases where we feel desperate because whatever we use doesn’t seem to work. In those patients, it seems very unlikely that you’re going to harm them by trying products like this. If you get a positive result, you’re going to be doing them a big favor and you’re going to feel good about giving them that product,” Dr. Hovanesian said.
Dr. Houser said that amniotic membrane might be a nice adjuvant though not always necessary in situations like autoimmune dry eye disease flares, which can respond well to amniotic membrane. However, it is important to initiate other long-term therapies such as autologous serum, cholinergic agonists, or anti-inflammatory drops in conjunction with amniotic membrane to prevent future flares.
“Especially in cases where we would like to heal the ocular surface quickly, such as patients having a flare from their baseline dry eye or patients in whom we are trying to optimize the ocular surface prior to cataract surgery and who can’t tolerate steroid drops, amniotic membrane can be a useful adjuvant treatment to other longer-term maintenance therapies,” she said.
While Dr. Houser thinks that amniotic membrane has a strong ability to heal the ocular surface, she doesn’t find it offers a lasting effect for patients with underlying structural abnormalities, such as epithelial basement membrane dystrophy.
“While amniotic membrane could provide some short-term relief from the irritation or dryness, the underlying structural abnormality still remains and will continue to cause visual symptoms or discomfort until surgically addressed with superficial keratectomy or phototherapeutic keratectomy,” she said.
About the physicians
Kourtney Houser, MD
Assistant Professor of Ophthalmology
Duke University School of Medicine
Durham, North Carolina
John Hovanesian, MD
Harvard Eye Associates
Laguna Hills, California
Relevant disclosures
Houser: None
Hovanesian: None
Contact
Houser: kourtney.houser@gmail.com
Hovanesian: johnhova@gmail.com