Glaucoma
March 2021
by Ellen Stodola
Editorial Co-Director

Source: Kateki Vinod, MD
EyeWorld spoke with several glaucoma specialists who discussed changes they’ve noticed in glaucoma as well as in their own practices due to the COVID-19 pandemic. They shared how they’ve adapted to continue patient care and described the changes they think are here to stay post-pandemic.
Changes in response to COVID-19
Sarwat Salim, MD, said that she has noticed tremendous collaboration and a multi-disciplinary approach to research, evidence-based medicine, education, advocacy, and the use of technology and telemedicine platforms in the past year. “It is wonderful to see how different organizations are partnering as we navigate the rapidly evolving COVID-19 crisis,” she said. “Each day we are learning, growing, and developing new strategies to protect our patients and staff and to ensure the best possible clinical practices and outcomes.”
Inder Paul Singh, MD, has noticed a change in patients in that they are carefully observing all the new requirements in the practice. They are watching staff actions and changes to protocols, like mask wearing and cleaning, he said. Dr. Singh thinks it’s important to maintain these protocols long term to protect patients, physicians, and office staff.
In Dr. Singh’s practice, the waiting room was reorganized for social distancing; technology is being used as a paging system; and patients can check in online or at a kiosk outside and they’re notified when the physician is ready. Dr. Singh said patients like waiting in their car until their appointment time. “I’ve heard patients say they don’t mind waiting a little longer in their car where they can sit back and listen to the radio,” he said.
MDbackline is a tool Dr. Singh has been using to reduce patient time in the office. Patients fill out questionnaires in advance, giving the doctor and technicians information (personality traits, motivation, and other history) without the technician needing to gather it face to face. “I have that information to make decisions or tailor my discussion with the patient before they come in,” Dr. Singh said.
Other technologies helping to minimize in-office time for the patient in Dr. Singh’s practice include VERACITY Surgical (Carl Zeiss Meditec), which allows the doctor and staff to use patient history, biometry, and diagnostic testing. Dr. Singh described FORUM software (Carl Zeiss Meditec) as a “way to manage all the diagnostic information acquired and consolidate it into one system, but [it] also allows AI to take over.” Finally, Dr. Singh said technologies such as the SL 800 slit lamp (Carl Zeiss Meditec), which has a telemedicine component, allows for remote access. If a technician or optometrist is performing a patient workup, the physician can view what’s happening from outside the office.
At Dr. Salim’s practice, patients and visitors are screened for COVID symptoms before coming in and again upon arrival. “We have a screening station at the entrance of the building where everyone is asked to clean hands with a hand sanitizer and is provided a mask.” Visitors and guests are limited, and Dr. Salim said some administrative staff continues to work remotely to reduce in-house volume. Like many practices, Dr. Salim’s clinic has installed Plexiglass at reception desks, removed magazines, rearranged waiting room furniture, instituted frequent disinfection protocols, and added signage that reminds of social distancing.
“We moved service-specific testing equipment to their respective clinics to limit patient movement between floors. We have also changed our workflow so that staff is moving around the patient versus having the patient move around the staff, and this change has helped decrease wait time,” she said.
COVID testing preop is recommended for patients who need surgery with general anesthesia, Dr. Salim said.
Enhanced infection control measures adopted at NYEE in spring 2020 are still in place today, Dr. Vinod said. “Patients visiting NYEE undergo a screening questionnaire regarding symptoms of COVID, exposure to infected or symptomatic individuals, and recent travel to ‘hot spots.”’
Outpatients are allowed one companion, if required for assistance with mobility or language translation. After having temperatures checked with non-contact, infrared thermometers, patients clean their hands with alcohol-based hand sanitizer and are provided surgical masks upon entry to the hospital. A second screening questionnaire is conducted once patients reach the ophthalmologist’s office. All staff undergo the same process upon arrival to work. Limited numbers of people are allowed in elevators and waiting rooms to allow for social distancing.
Dr. Vinod said clinic flow was adjusted to streamline patient visits and minimize time spent in the waiting room between technician workup and the ophthalmologist’s evaluation. Slit lamps have breath shields, and all high-touch surfaces and diagnostic equipment are thoroughly disinfected between patients using EPA-registered disinfectants.
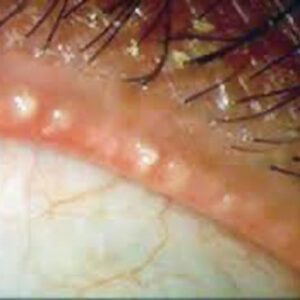
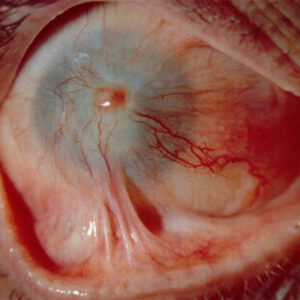
With patients required to wear surgical masks for the duration of their visit, paper tape is used to seal the top edge of the mask to prevent fogging of the lens and minimize artifacts during perimetry, Dr. Vinod said. “We’ve been using disposable gonioprisms and Goldmann applanation tonometer tips,” Dr. Vinod said. “Our non-glaucoma colleagues prefer the iCare and Tono-Pen tonometers [Reichert Technologies] to check IOP, which employ single-use probes and tip covers, respectively. We’re also using disposable lenses for our laser procedures.”
She added that all patients scheduled for ambulatory surgery at NYEE are required to undergo COVID testing within 5 days of their surgical procedure. Visitors are not permitted within the preoperative or postoperative areas. Companions are asked to wait in designated areas with seating arranged to allow for 6-foot social distancing. Surgeries for patients who test positive for COVID are either postponed or, if urgent, performed in a dedicated OR, typically at the end of the day to allow for terminal disinfection. Surgeons and staff wear N95 respirators in the OR.
Early months of the pandemic
Dr. Salim said that her practice remained open to provide in-person services to urgent and emergent patients. “We also started using telehealth platforms for routine patients to ensure continuity of care,” she said.
“Other than providing ophthalmic care, we were deployed to a COVID testing center where hundreds of patients were screened daily for the virus. We were extremely fortunate to have adequate PPE for all physicians, nurses, and staff at the testing center,” she added. “It was gratifying to serve the community and demonstrate our collective resolve and strength during these difficult times.”
NYEE also remained open, though Dr. Vinod noted modifications to all aspects of daily operations. “Our hospital is a major hub for ophthalmic care not only for the five boroughs of New York City but also the tri-state area and beyond,” she said. “As such, we remained open even at the height of the pandemic to provide urgent and emergent glaucoma care when routine visits and elective surgery were being postponed throughout the region.”
Brian Francis, MD, said that his practice only saw emergent cases when the pandemic began. Regular checks were postponed, but the practice still saw those with high pressures or those who were unstable. His practice did not transition to drive-thru IOP checks. Dr. Francis said this did not work logistically, but he noted that there was an effort to make visits quick and socially distanced.
Telemedicine
At the height of the pandemic, Dr. Vinod embraced teleophthalmology as a way to deliver routine glaucoma care.
“Telemedicine visits for glaucoma have proven useful in my practice for reviewing medications and their instructions for use, assessing adherence to and adverse effects from eye drops, and counseling patients about their diagnosis and management plans.”
However, Dr. Vinod noted that glaucoma management relies heavily on in-person diagnostic evaluation/testing. Although some tools are available for remote monitoring, most are still in early stages of development or haven’t been adequately validated.
Dr. Singh finds the “hybrid” telemedicine appointments particularly useful. During the early stages of the pandemic, he said his practice relied heavily on telemedicine, but even with a return to office-based practice, he still finds it a useful tool for triaging patients. With this model, patients see technicians for in-person diagnostic tests, then Dr. Singh follows up later on a call to discuss.
“Patients love having the time online to do telemedicine,” he said. “They think it’s more intimate with the doctor not being in the office.” He added that his practice will continue to maintain some form of telemedicine going forward, particularly for those patients who are stable.
“I think telemedicine will help triage our patients better,” Dr. Singh said. For example, he said that for post-surgery patients, it’s helpful to do a telemedicine visit if the patient is experiencing a complication to determine if the patient needs to be seen immediately, within a day, or later.
“There’s no doubt that because the regulations and coding have been improved, it makes it more palatable to offer telemedicine,” he said.
Visual field testing
“While virtual visits offer an opportunity to connect with the patients, facilitate history taking, assist in addressing queries or concerns, and allow a limited anterior segment examination, we are unable to measure IOP, assess the optic nerve, or perform perimetry,” Dr. Salim said. “Home-based tonometers are limited by their suboptimal accuracy and cost. Portable alternatives to standard automated perimetry, web-based visual field programs, and virtual reality-based visual field testing have been developed. However, additional data and experience are needed to further assess their reliability and feasibility before their use at home.”
Dr. Salim said her clinic still measures IOP using Goldmann applanation tonometer and evaluates visual function with a standard visual field analyzer. “Sometimes we offer testing on separate days to minimize the total contact time for patients in the clinic.” Depending on the stage of glaucoma, she may order OCT and visual field on separate days and rely more on the clinical examination to tailor treatment.
Telemedicine does not take the place of a physical exam, Dr. Singh said, though it helps when you can’t see the patient. “We still have to do gonioscopy and look at the nerve physically,” he said. Dr. Singh added that visual field testing at home should be more available in the future, which would “change the paradigm if we could evaluate the patient at home.”
Sustained drug delivery
Dr. Francis said he is using sustained drug delivery devices more so because they are new technology rather than because of the pandemic. “I wouldn’t necessarily say that they helped patient management that much during the pandemic,” he said. “If you’re trying to control pressure and not have to do surgery, it can be helpful in that regard. Also, if you have a patient that relies on caregivers for medication but may have this care disrupted due to the pandemic, a drug delivery system ensures they remain adequately treated. But in terms of patients getting medication, if they are able to use the medication properly, we’ve been able to easily get it to them due to home delivery,” he said.
Dr. Salim said that Durysta (bimatoprost implant, Allergan), the first FDA-approved sustained-release biodegradable implant, is a great addition and has the potential to overcome compliance issues, reduce the treatment burden, and minimize tolerability concerns. “This may be a good option for some patients who are uncomfortable coming to the office during the pandemic,” she said. “At this point, we are still gaining more experience with this new implant, and I think its use should be tailored to each patient’s clinical situation and social circumstances.”
Pandemic’s impact on number of patients, time spent with patients, frequency of visits
“Given the insidious and asymptomatic nature of glaucoma, delaying follow-up can be risky,” Dr. Vinod said. Many New Yorkers rely on public transportation and have to take multiple trains/buses to get to NYEE. “My patients were faced with what seemed like an impossible choice at the height of the pandemic when stay-at-home orders were in place: delay their glaucoma care and risk disease progression or keep their in-person appointments and risk exposure to SARS-CoV-2 while traveling to/from the office.”
Additionally, the fear of entering a hospital (even a subspecialty one that did not treat COVID patients such as NYEE) contributed to the reluctance to attend office visits, she said.
Increasing the intervals between visits is a consideration for glaucoma suspects or patients with excellent adherence and stable disease. However, Dr. Vinod said many of her patients have advanced glaucoma with multiple ocular comorbidities, requiring frequent and vigilant follow-up.
“Teamwork among our administrative staff, ophthalmic technicians, and physicians has been of paramount importance in instituting infection control measures and maintaining a safe and reassuring environment for our patients,” she said. “Many modifications to the delivery of glaucoma care, such as those we have incorporated at NYEE, will remain in place indefinitely as part of this ‘new normal.’”
Dr. Salim has found that her clinical and surgical volume has decreased. “With increased resurgence of COVID-19 cases, many patients are either canceling appointments or not showing up to their scheduled visits,” she said. “We have a system in place to reach out to these patients to offer telemedicine to ensure continuity of their care. With time, we hope that more patients will keep their clinic appointments.”
Dr. Salim is scheduling in-person appointments further out for patients with stable disease. For advanced glaucoma patients, more frequent follow-up is still warranted.
“I am doing more 90-day prescription refills for patients already on medications,” she said. “For the new patients, I discuss details of the LiGHT trial and more readily offer laser to minimize cost, avoid compliance issues, reduce IOP fluctuations, and decrease the total number of visits. I continue to offer telemedicine to patients who are either at a higher risk of developing infection or are not comfortable coming to the hospital.”
Dr. Francis said he thinks changes in patient numbers and the way practices operate will still be in effect for the foreseeable future. He said his practice has been figuring out how many patients they can have on the schedule and how to space them out to keep the waiting room socially distanced. “We figured out that our time for one patient needs to be less than an hour,” he said, from check-in to check-out.
Dr. Francis said his practice is operating around 80% volume, which he expects to continue. “We’re spacing out appointments a little more,” he said, adding that if a patient is stable, he might wait longer between appointments. A time-saving tip Dr. Francis offered is to plan and prepare which tests will be performed before the patient comes in rather than on the spot.
ARTICLE SIDEBAR
How has COVID-19 impacted training programs in the United States?
Dr. Salim discussed how the pandemic affected medical students, residents, and fellows. During the height of the pandemic, many rotations for medical students were canceled, and many academic centers stopped electives for out-of-state students. “As a result, many students were not able to acquire the typical clinical and research experiences, find mentors to provide career counseling or write letters of recommendation, or explore programs for residency,” Dr. Salim said. “These limitations also presented challenges for educators in terms of screening the most qualified candidates for their specialties.”
With decreased clinical volume, the surgical experience was affected for many residents and fellows. However, Dr. Salim said that the didactic lectures increased. “It has been wonderful to witness increased communication and collaboration across various academic programs.”
Some fellows had difficulty securing a good job while others faced delays in their start dates with new employment, she said, adding that some had to work around the negotiations of original contracts given the profound impact of COVID-19 on practices.
“Despite numerous challenges, I think COVID-19 has pushed us to think differently. We are developing innovative methods and solutions to educate and certify the next generation of physicians,” Dr. Salim said. “I have had the privilege to serve as an examiner for the American Board of Ophthalmology for the past several years. The virtual oral board exams were highly successful this year and also cost effective. Both the candidates and examiners participated in the exams over the weekends and did not have to take time off from their clinical responsibilities.”
About the physicians
Brian Francis, MD
Doheny Eye Institute
UCLA Geffen School of Medicine
Los Angeles, California
Sarwat Salim, MD, FACS
Professor of Ophthalmology
Director, Glaucoma Service
New England Eye Center of Tufts University Medical Center
Boston, Massachusetts
Inder Paul Singh, MD
The Eye Centers of Racine and Kenosha
Racine, Wisconsin
Kateki Vinod, MD
Assistant Professor of Ophthalmology
Icahn School of Medicine at Mount Sinai
New York Eye and Ear Infirmary of Mount Sinai (NYEE)
New York, New York
Relevant disclosures
Francis: None
Salim: Aerie Pharmaceuticals
Singh: Carl Zeiss Meditec
Vinod: None
Contact
Francis: bfrancis@doheny.org
Salim: ssalim@tuftsmedicalcenter.org
Singh: ipsingh@amazingeye.com
Vinod: kate.vinod@gmail.com