Cornea
December 2020
by Maxine Lipner
Senior Contributing Writer
When teens come into the clinic, it’s important to consider that they might have dry eye or meibomian gland disease. Investigators in a recent study found that among minors coming in for eye exams, 15% were experiencing dry eye discomfort and 9% had signs of meibomian gland dropout, according to lead investigator Anna Tichenor, PhD.1
“We were expecting that their meibomian glands would be healthy and everything would look great,” Dr. Tichenor said. The fact that so many were reporting discomfort was surprising, Dr. Tichenor added, but noted that the meibomian gland dropout rate was not statistically significant.
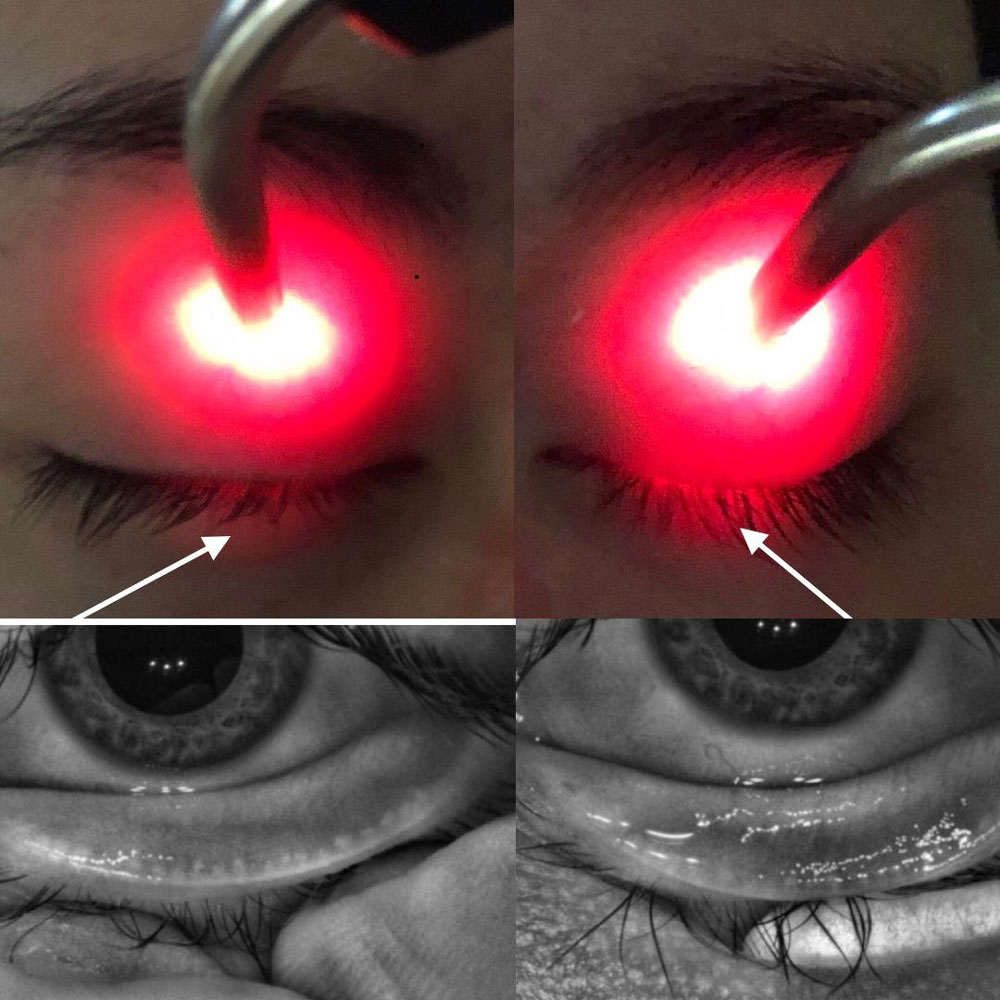
Source: Laura Periman, MD
The study included 225 individuals 8–17 years old. Among older individuals (14–17 years old), dropout rates rose to 11%, Dr. Tichenor reported, speculating that it could be due to digital device use.
“We started to hear potential links with digital devices and dry eye,” she said. Though the research did not find a significant association with device use and dry eye, it’s possible that the dry eye was not yet severe enough and a link may have been seen in slightly older patients, Dr. Tichenor said. When it comes to dropout, it’s unclear whether some amount may be normal. Approximately 30 of the subjects said they used mascara, but no correlation was found. “I think that’s because there was such a small number of them who used makeup,” Dr. Tichenor said.
Other studies have identified dry eye among younger patients, too. Laura Periman, MD, cited a study that showed the majority of young patients have at least a mild degree of meibomian gland atrophy, with moderate and severe disease also present in some.2
In Dr. Periman’s view, significant dry eye risk factors for teens are screen time and use of acne care products. “These things are known ocular surface offenders,” she said. One study showed that those who used isotretinoin/erythromycin had a decreased tear film breakup time and lower ocular surface disease index scores, Dr. Periman noted.3 Fifty-one percent of eyes also had punctate epitheliopathy.
It’s not enough for patients to avoid the eye area when applying these products. “They’re not putting it anywhere near the orbital rim because you don’t get pimples there,” Dr. Periman said, adding that there was either a migration effect or downregulation of meibum in the neighborhood in response to these drying medications.
Trendy cosmetics can also cause dryness. Instagram is full of cosmetic tutorials, Dr. Periman noted. “I cringe when I see these,” she said. One such technique involves applying eyeliner directly on the lid margin, known as tightlining. “That can effectively block your meibum flow,” she said.
Some teens may also do eyelash perming, she continued. With this, a plastic bolster is used and solution is placed on the base of the eyelashes to permanently crimp them. This interferes with the eye’s natural defense in which the lashes are in a certain position to maximize the deflection of wind, allergens, and debris. Eyelash growth serums are proinflammatory, Dr. Periman continued, and make the meibomian glands sick.
Cynthia Matossian, MD, cited teens’ propensity to try the latest beauty trends as troubling. “Lash extensions are very popular these days. The glues that are used to adhere the individual extension onto natural lashes is not good for the ocular surface,” Dr. Matossian said. “The fixatives may contain latex and other chemicals that can cause surface irritation or allergic blepharoconjunctivitis.” Also, the extreme length of the lashes can be a problem. Instead of repelling debris, these abnormally long lashes can create a reverse air current where pollutants, pollen, and micro-debris get propelled onto the tear film. False lashes are even more damaging since the glued-on lash strip has to be removed on a daily basis. The process of peeling off the false eyelashes along with the weight of the extreme lashes may lead to permanent lash loss and traction alopecia, Dr. Matossian warned.
Ingredients in makeup as well as moisturizers and concealers can also dry the eye. “Many of them contain paraben and other ingredients that are very irritating to the ocular surface and tear film,” she said.
“Teenagers are notorious for overwearing their contact lenses and not properly cleaning them,” Dr. Matossian said. “They sleep in them, they swim in them, and they go in the hot tub in them.” All of this inappropriate use leads to stress on the ocular surface.
Dr. Matossian said she thinks digital devices play a role in dry eye. “This is the first generation to grow up with electronic devices starting when they were toddlers,” she said. “It’s taking a toll on the ocular surface.” She attributes this to a decreased blink rate from approximately 20 blinks per minute to around four. “The upper and lower lids are supposed to ‘kiss’ each other with each blink,” Dr. Matossian explained. This action releases a small quantity of olive oil-like meibum from the meibomian glands to coat the surface of the eye. If there is an inadequate or incomplete blink, the lipid is not released on a regular basis. The meibum congeals to a more viscous consistency and causes impaction of the meibomian gland, leading to permanent dysfunction.
Addressing dry eye in teens may involve educating pediatricians to refer them for regular eye examinations, Dr. Matossian said. Unless teens take care of their glands, they may end up with more complications as they reach adulthood, Dr. Matossian concluded.
About the doctors
Cynthia Matossian, MD
Matossian Eye Associates
Doylestown, Pennsylvania
Laura Periman, MD
Director of Dry Eye Services and Clinical Research
Oracle Eye Institute
Seattle, Washington
Anna Tichenor, PhD
Assistant Professor
Indiana School of Optometry
Bloomington, Indiana
References
- Tichenor AA, et al. Tear film and meibomian gland characteristics in adolescents. Cornea. 2019;38:1475–1482.
- Gupta PK, et al. Prevalence of meibomian gland atrophy in a pediatric population. Cornea. 2018;37:426–430.
- Aslan Bayhan S, et al. Effects of topical acne treatment on the ocular surface in patients with acne vulgaris. Cont Lens Anterior Eye. 2016;39:431–434.
Relevant disclosures
Matossian: None
Periman: None
Tichenor: None
Contact
Matossian: cmatossian@matossianeye.com
Periman: lauraperiman@yahoo.com
Tichenor: aablamow@uab.edu



