Cornea
March 2021
by Ellen Stodola
Editorial Co-Director
With more than 1 million new cases each year, herpes zoster is increasing in frequency, according to Vincent de Luise, MD. As the population ages, the incidence increases, with an incidence of 1 in 3 overall and 1 in 2 in those over age 85. Dr. de Luise stressed that prompt diagnosis is essential, and systemic antivirals are required to reduce the viral load and reduce the incidence of post-herpetic neuralgia.
Dr. de Luise and Elisabeth Cohen, MD, spoke to EyeWorld about the vaccine for herpes zoster that is now available, how to manage various complications associated with herpes zoster, and treatment options.
Status of vaccines
Shingrix (GlaxoSmithKline) is widely available now, Dr. Cohen said, adding that it may be more available at chain pharmacies than in doctors’ offices.
“The new one is much more effective and safer because it doesn’t contain a live attenuated virus,” she said. “In the U.S., there are not people who would be better off with the original vaccine, which is less effective and does have the risk of attenuated virus, which is a real risk in people who are immunocompromised.”
The Shingrix vaccine is FDA approved and is indicated for those 50 and older. Immunocompromised patients were not included in the landmark studies, Dr. Cohen said, but there have been a number of papers since then showing that the vaccine is safe and effective in a variety of immunocompromised populations. “You don’t have to worry about safety with regard to infection; there may be potential safety issues with regard to stimulating the immune system in people who have had transplants, but this has not been reported to date,” she said.

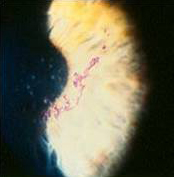
Source (all): Vincent de Luise, MD
According to GlaxoSmithKline, there had been regional shortages in the last few years, but at this time, there are sufficient quantities, Dr. de Luise said.
“The Shingrix vaccine is covered in some insurance plans as a preventative healthcare benefit,” he said. “Study data has demonstrated that the Shingrix vaccine stimulates production of specific immune memory cells (CD4 T cells), generating strong and sustained protection against the virus, with a 24-fold increase in CD4 T cell response, significantly more than the older Zostavax [Merck] vaccine. The Shingrix vaccine efficacy lasts at least 4 years and likely longer.”
Dr. de Luise noted that as of July 1, 2020, Merck stated that it will no longer produce the Zostavax vaccine. Doses of Zostavax at pharmacies and clinics could have been used up until Nov. 18, 2020, so Shingrix is now the only vaccine for herpes zoster.
Dr. de Luise said the Shingrix vaccine, given in two doses, is more than 90% protective effect against VZV, whereas Zostavax was only 51% effective in preventing disease. This also translates to a much higher rate of prevention against post-herpetic neuralgia for Shingrix than Zostavax, he said. Protection stays above 85% for at least the first 4 years.
The two Shingrix injections are spaced 2–6 months apart. Side effects include pain and malaise for several days, especially in persons less than age 70.
Should patients who have had herpes zoster receive Shingrix?
According to Dr. de Luise, patients can receive Shingrix even if they’ve had a prior episode of herpes zoster.
“Having had herpes zoster means that one has been exposed to wild-type virus,” he said. “That produces a natural immune response.” This natural immune response, largely a T cell response, usually lasts for several years and eventually decays. “If one wishes to receive the Shingrix vaccine, even if one has had a case of herpes zoster, the recommendation is to wait at least 3 months after an active herpes zoster infection to receive the vaccine,” Dr. de Luise said.
Dr. Cohen encouraged those who have had a herpes zoster episode to get the Shingrix vaccine. The purpose of the vaccine would be to prevent another episode in a different location, she said. “There isn’t as much immunity after an episode of herpes zoster as we thought in the past,” she said. “We used to think you could wait 1–3 years after an episode before getting vaccinated.”
Dr. Cohen noted that if a patient had an episode of zoster in the eye, it’s important to wait until the eye is stable before vaccination and be examined before and 3–6 weeks after each shot.
Neurotrophic changes of herpes zoster ophthalmicus (HZO) keratitis
Dr. Cohen said neurotrophic changes associated with herpes zoster keratitis may be less common with better antiviral treatment of acute disease. She suggested avoiding toxic medications and using lubricating drops and ointment. Tarsorrhaphy can be effective, though she added that this option is not necessarily popular with patients.
Some find Oxervate (cenegermin-bkbj, Dompe) helpful, but this option is expensive, Dr. Cohen said.
She added that a PROKERA (Bio-Tissue) amniotic membrane graft can be used when you have an ulcer from neurotrophic keratopathy. Neurotrophic keratopathy is serious because there can be melting and perforation of the cornea, as well as microbial super-infection, she said.
The neurotrophic consequences of HZO are the most ominous and potentially visually significant of the protean corneal sequelae of HZO, Dr. de Luise said.
“To diagnose HZO neurotrophic keratopathy requires vigilance and a high degree of suspicion,” he said. “Once diagnosed, there must be a rapid taper and cessation of any topical steroids that might be on board and the immediate institution of strategies that promote epithelial healing.” These include non-preserved artificial tear gels, autologous serum tears, and Oxervate.
According to Dr. de Luise, short-term use of a bandage contact lens with topical antibiotic coverage should only be employed with caution in neurotrophic keratopathy. If there is not a rapid response, then amniotic membrane graft, bridge conjunctival flap, or lateral tarsorrhaphy should be considered.
Oral antivirals
Dr. Cohen suggested that everyone receive a 7- to 10-day course of high-dose oral antivirals within 3 days of rash onset. This is approved and recommended, she said.
Dr. Cohen also mentioned the Zoster Eye Disease Study (ZEDS), a large NIH/NEI-supported randomized clinical trial she leads that is evaluating whether prolonged low-dose antiviral treatment reduces chronic and recurrent eye disease and/or post-herpetic neuralgia and should be the new standard of care. She said there is not currently good quality data on this subject.
In contrast, antiviral treatment is known to be safe, effective, and the standard of care for herpes simplex eye disease, caused by a related but different herpes virus. “Our study seeks to find out if that’s the case with HZO caused by the varicella zoster virus as well,” Dr. Cohen said. The study will include centers across the U.S., Canada, and New Zealand.
Timeline for oral antivirals after dermatological eruption
Dr. de Luise said that even if a patient presents more than 72 hours after having had the cutaneous eruption, it is still strongly recommended to give a full, 1-week course of an oral antiviral, acyclovir, famciclovir, or valacyclovir.
Dr. Cohen said that oral antivirals can be used if the patient still has an active rash, but if it is scarred or scabbed over, you might not want to use these antivirals.
Are oral steroids ever indicated in HZO management?
Dr. de Luise said that two large, controlled studies from the 1990s evaluated the addition of oral corticosteroids to acyclovir therapy. Compared to antiviral agents alone, the combined regimen was found to accelerate the resolution of acute neuritis and provided an improvement in quality of life metrics.1,2
Dr. de Luise added that in immunocompromised hosts or in patients with diabetes mellitus, oral steroids can rarely cause viral dissemination by lowering the immune response. If oral steroids are to be used in the management of HZO, it’s recommended to reserve them for severe cases with acute pain along with the cutaneous eruption; use lower doses, initiate therapy a few days after oral antivirals, and discontinue oral steroids after completing oral antivirals. The oral antivirals lower the viral load and the risk of viral dissemination if the oral steroids are added.
Dr. Cohen discussed the “controversy” about the use of oral steroids. “Generally, they’re used less than in the past,” she said. She thinks steroids are indicated if you have involvement of the optic nerve or orbital inflammation, “but most of the time for herpes zoster ophthalmicus, we do not use oral steroids,” she said. There is some evidence that they might reduce acute pain but no long-term benefit, and there is a risk that they could make infection worse. She said patients should be on antivirals if they’re taking oral steroids during the zoster episode.
Topical corticosteroids for HZO anterior segment disease
Topical corticosteroids are used frequently in HZO, Dr. Cohen said, and many people may have to be on a low dose for a long time because if you go below a certain amount, the eye disease will flare up. Dr. Cohen said that she had HZO in 2008 and still needs a low dose of topical steroids a few times a week to prevent recurrent inflammation in the eye.
Topical corticosteroids in HZO anterior segment disease should be used only for corneal and anterior segment manifestations with inflammatory etiology, Dr. de Luise said, such as disciform keratopathy, stromal keratitis, and iridocyclitis. “Topical corticosteroids do not have efficacy in the setting of pleomorphic, wandering epithelial HZO keratitis and are contraindicated in HZO epithelial keratitis in patients with HIV/AIDS,” he said.
IV antivirals
Immunocompromised hosts have a much higher likelihood of systemic viral dissemination and should be monitored carefully, with strong consideration of IV antivirals, Dr. de Luise said, adding that IV acyclovir is the first choice. IV foscarnet is the drug of choice in acyclovir-resistant herpes zoster, he said.
Dr. Cohen said that IV antivirals are often used if you have neurologic involvement at the onset, and she said that you have to be aware that HZO is a risk factor for having a stroke, especially within the first month. IV antivirals are used when there is central nervous system involvement or involvement of cranial nerves or the orbit.
Management of HZO-related IOP rise and glaucoma
People with HZO can have problems with secondary glaucoma caused by a variety of mechanisms, Dr. Cohen said.
“If one has iritis or inflammation inside the eye, that is often associated with very high pressure and can result in rapid onset of glaucoma, visual field loss, and optic nerve damage,” she said. Additionally, steroids used to treat topical inflammation can cause elevated pressure and risk for glaucoma. Anyone on topical steroids should be monitored closely for glaucoma, she added.
The mechanisms of IOP rise and glaucoma in HZO include trabeculitis, synechial scarring in the angle, use of topical corticosteroids beyond 3 weeks, and mechanical blockage of the trabecular meshwork by inflammatory cells, Dr. de Luise said.
“Management should be initiated with aqueous suppressant medications,” he said. “Topical corticosteroids should also be employed, always with careful and frequent follow-up.” He added that concerns about corticosteroid-induced IOP are valid but are tempered by the fact that topical corticosteroids are essential for inflammatory glaucoma management.
Additionally, Dr. de Luise said that topical prostaglandins have long been debated in inflammatory glaucoma management.
“While there have been rare case reports of topical prostaglandins inducing CME in cases of inflammatory glaucoma, their use should still be considered in these cases,” he said. “If medication strategies fail, filtration surgery or tube/shunt is recommended.”
Dr. Cohen said that she strongly recommends vaccination with Shingrix for persons age 50 years and older, per the FDA approval.
ARTICLE SIDEBAR
Should ophthalmologists manage post-herpetic neuralgia in HZO?
According to Dr. de Luise, post-herpetic neuralgia (PHN) is defined as pain that persists after the first 4 weeks of the cutaneous eruption or pain that presents after the first 4 weeks of the cutaneous eruption. PHN can be a difficult and at times prolonged and intractable sequela of HZO. It is generally best if the ophthalmologist refers patients with PHN to a neurologist, neuro-ophthalmologist, or pain management anesthesiologist, he said.
“Ophthalmologists can consider initiating therapy for milder cases of PHN, with strategies such as the tricyclic antidepressant amitriptyline, which also has some pain-relieving properties, or 5% lidocaine patches to the affected skin area,” Dr. de Luise said. “The calcium channel alpha 2 delta ligand oral agents gabapentin and pregabalin are both FDA labeled for PHN.”
If PHN persists, it is strongly recommended to enlist neurologists and/or pain management specialty anesthesiologists for further strategies, which can include opioids and stellate ganglion block, Dr. de Luise said.
Dr. Cohen agreed that it’s helpful to work with a pain management group and/or a neurologist if this issue occurs, as they may be more comfortable prescribing the necessary medications.
Post-herpetic neuralgia is the most common and serious complication of zoster. It occurs more frequently in older patients, she said, and can have a terrible impact on quality of life. Additionally, Dr. Cohen said that zoster is a risk factor for new onset of depression and is also a common cause of suicide due to pain in people age 70 and above. “If you can’t control the post-herpetic neuralgia using a reasonable dosage of neuropathic pain medicines or anti-depressants, it’s important to work with neurologists and pain management specialists to enhance quality of life for patients and minimize use of narcotic pain medicines as much as possible,” she said.
She again stressed that she strongly recommends vaccination with Shingrix for persons age 50 years and older, per the FDA approval.
About the physicians
Elisabeth Cohen, MD
Professor, Department of Ophthalmology
NYU Grossman School of Medicine
NYU Langone Health
New York, New York
Vincent de Luise, MD
Assistant Clinical Professor of Ophthalmology
Yale University School of Medicine
New Haven, Connecticut
References
- Whitley RJ, et al. Acyclovir with and without prednisone for the treatment of herpes zoster. A randomized, placebo-controlled trial. Ann Intern Med. 1996;125:376–383.
- Wood MJ, et al. A randomized trial of acyclovir for 7 days or 21 days with and without prednisolone for treatment of acute herpes zoster. N Engl J Med. 1994;330:896–900.
Relevant disclosures
Cohen: None
de Luise: None
Contact
Cohen: Elisabeth.Cohen@nyulangone.org
de Luise: vdeluisemd@gmail.com



