Cover Feature: Corneal diagnoses and systemic disease
April 2012
by Enette Ngoei
EyeWorld Contributing Editor
Telling the difference between Mooren’s ulcer and early signs of something deadly
While Mooren’s ulcer is by definition not associated with any systemic autoimmune disorder, it can be confused with corneal ulcers that are early warning signs of life-threatening diseases, said C. Stephen Foster, M.D., founder and president, Massachusetts Eye Research and Surgery Institute, Cambridge, and clinical professor of ophthalmology, Harvard Medical School, Boston.
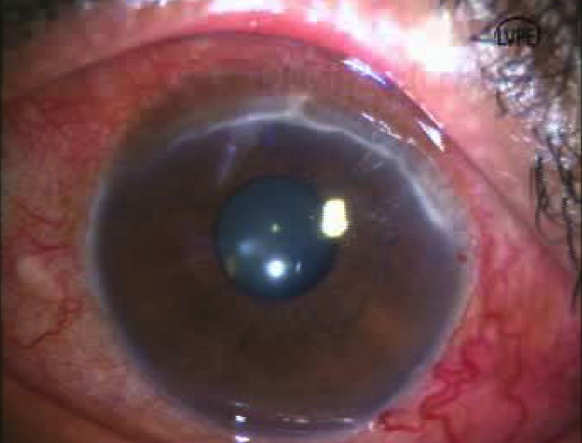
Therefore, the general ophthalmologist ought to hear alarm bells ring if the peripheral corneal disease has the following characteristics: It is a real ulcer, that is, the epithelium is not intact, there is some loss of stroma, it is a real keratitis, so inflammation is present, and white blood cells have infiltrated into the peripheral cornea. This, by definition, is peripheral ulcerative keratitis (PUK), Dr. Foster said.
According to Prashant Garg, M.D., L.V. Prasad Eye Institute, Hyderabad, India, “In ulcerative processes, if the ulcers are primarily located at the periphery of the cornea and there is no separation, it becomes an indicator that you should investigate for collagen vascular diseases.”
PUK is caused by a limited number of things, Dr. Foster said. For example, if a patient has peripheral keratitis and there are white blood cells infiltrated into the stroma, that may just be a hypersensitivity reaction to staphylococcal protein, not PUK.
“If you cling to the definition that I laid out for PUK, now you’ve got a person who might have Mooren’s ulcer or alternatively might have the peripheral corneal disease as a consequence of a potentially lethal systemic vasculitis; those diseases include granulomatosis with polyangiitis (Wegener’s), polyarteritis nodosa, and then a couple of the other classic rheumatologic disorders,” he said.
Distinguishing between Mooren’s disease and PUK
The characteristics of PUK and Mooren’s ulcer are very much the same as the characteristics in a person with polyarteritis or granulomatosis with polyangiitis, or relapsing polychondritis or rheumatoid disease, Dr. Foster said.
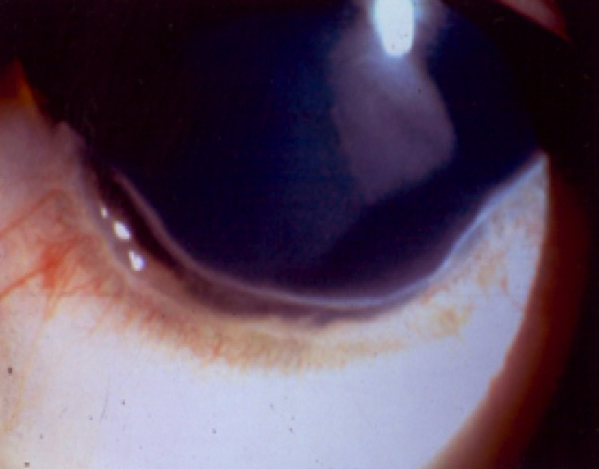
The characteristics include an ulcer progressing slowly and easily, circumferentially, and deeper toward the center of the cornea. If one uses a fine instrument to explore the ulcer, one will find that it has an overhanging lip; if this fine instrument is exploring the ulcer toward the center of the cornea, one can be absolutely astonished at how far into the cornea the instrument can go before it meets resistance. In other words, there’s a lot more destruction than is clinically apparent at the slit lamp, Dr. Foster said.
Therefore, a very thorough systemic evaluation is mandatory in any patient that is believed to have Mooren’s ulcer, Dr. Foster said.
In fact, the diagnosis should be PUK from the beginning; then, if the aggressive systemic evaluation is negative and the adjacent sclera is not involved, it’s appropriate to hang the label Mooren’s ulcer on this patient, he said.
Dr. Foster added, “The systemic evaluation should not discover that the patient has an elevated C-reactive protein, an elevated sedimentation rate, auto-antibody production of any type but particularly antineutrophil cytoplasmic antibody.”
If it’s Mooren’s ulcer, the systemic prognosis is excellent. Otherwise, aggressive systemic immunomodulatory medication is mandatory if the patient’s PUK is found to be a consequence of polyarteritis nodosa or microscopic polyangiitis and granulomatosis with polyangiitis, he said.
“If not treated, the patient will die,” he said.
Source (all): Virender S. Sangwan, M.D.
Treating Mooren’s ulcer
A patient with unilateral Mooren’s ulcer may do just fine with the removal of the adjacent conjunctiva, Dr. Foster said.
Virender S. Sangwan, M.D., associate director, L.V. Prasad Eye Institute, agreed: “The overall prognosis is good if it’s treated in a stepwise manner. In 70-80% of the patients, you can save their eyesight or the globe.”
He continued, “Essentially the first step that we take for these patients is conjuctival resection in the area of involvement within 1 clock hour on either side of the whole area followed by tissue adhesive application with intense topical steroids.”
Medical treatment would not be sufficient for most of the Mooren’s ulcer patients unless it’s very mild, like less than 1 or 2 clock hours; then the physician can try intense topical steroids like prednisolone acetate, Dr. Sangwan said. Many of these patients will also need systemic steroids and immunosuppressants, he added.
There is also a bilateral form of Mooren’s ulcer, Dr. Foster said.
“If [the patient has] it in both eyes, things change. The odds of a conjunctival resection and aggressive topical steroid use putting the problem into remission go way down. In those bilateral cases, it’s very common to need systemic immunosuppressant chemotherapy,” he said.
While there have been some reports linking Mooren’s ulcer with hepatitis C, according to Dr. Sangwan, “There is no consensus on this issue as there are only a few case reports that talk of association, and no good prospective study has shown this to be true.”
Most of the experts in the corneal area do not believe in such an association and don’t treat these patients with anti-hepatitis treatment, he added.
Along similar lines, Dr. Foster said Mooren’s ulcer is by definition not associated with any systemic autoimmune disease; however it may be triggered by a myriad of things including infection like hepatitis C, salmonella, and intestinal parasites.
“One must take a proper history and do diagnostic tests and then move along therapeutically. Treat systemically as indicated. An infectious disease specialist should assess and render an opinion about interferon therapy or otherwise for the hepatitis C,” he added.
All of these diseases require the support of the internist, Dr. Garg said.
“It is important that we work closely with the internist, for the care of the general health and ocular management is only successful if the systemic disease is brought under control,” he said.
Editors’ note
The doctors mentioned have no financial interests related to this article.
Contact information
Foster: 617-797-0849, sfoster@mersi.com
Garg: 91-40-3061-2446, prashant@lvpei.org
Sangwan: 91-40-3061-2632, vsangwan@lvpei.org



