Cover Feature: Challenging cataract cases
October 2010
By Michelle Dalton
EyeWorld Contributing Editor
Presenting with a “completely dilated and non-reactive” pupil on post-op day 1 can be nerve-wracking for the surgeon … Here’s how one physician dealt with the complication
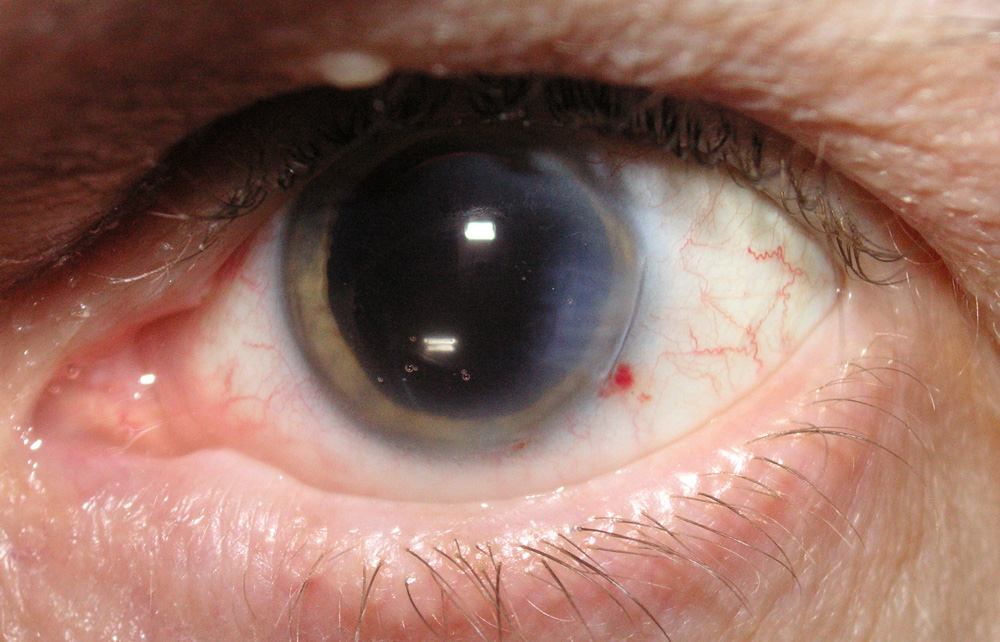
When it comes to cataract surgery, minor inconveniences, such as pupils that do not dilate well, add a bit more stress for the surgeon, but are by no means insurmountable obstacles to performing the surgery. And in cases where the first eye dilates poorly but the surgery is uneventful, surgeons are prepared for the second eye to also dilate poorly. So when a 78-year-old male who had undergone routine uncomplicated clear cornea phaco under topical anesthesia presented on post-op day 1 with a completely dilated and non-reactive pupil in the operated eye, Ernesto Collazo, M.D., San Juan, Puerto Rico, was concerned. The patient’s uncorrected visual acuity of 20/200 only pinholed to 20/50. Intraocular pressure was 16 mm Hg, the cornea was clear and the patient had minor cell and flare (+1) in the 12-24 hour post-op period, Dr. Collazo said. “There was no stromal edema or the epithelial microcystic edema one would expect to see after a prolong episode of high IOP. This was his second surgery with me; his first cataract operation had been 3 years earlier, and there were no post-op complications,” said Dr. Collazo. “This was a compliant patient, who denied using any drops other than the prescribed Pred Forte [prednisolone acetate, Allergan, Irvine, Calif.], Acuvail [ketorolac 0.45%, Allergan], and Zymar [gatifloxacin, Allergan].”
Potential causes
A permanent, dilated non-reactive pupil “can be caused by very high post-op pressures due to retained viscoelastic,” said Luther L. Fry, M.D., Garden City, Kan. In that instance, however, “I would expect the patient would have had some pain and nausea in the evening of the surgery.”
Increased IOP overnight “could damage the iris sphincter and one finds a widely dilated, non-responsive pupil afterwards. This would typically only occur with very high IOPs that should normally alert the patient with symptoms of ocular pain and/or headache,” said Arthur Cummings, F.R.C.S.Ed., medical director, Wellington Eye Clinic, Dublin, Ireland. “By the time the patient was seen the next day, the IOP could have returned to normal while the sphincter damage is still present.”
When an eye diffusely dilates like this patient’s eye did, “you have to rule out that atropine was given. In a really busy surgical center, where the bottles of dilating drops have red caps on them, someone could have grabbed the atropine by mistake,” said Nick Mamalis, M.D., professor of ophthalmology, John A. Moran Eye Center, Department of Ophthalmology & Visual Sciences, University of Utah, Salt Lake City. If the problem was caused by atropine, Dr. Mamalis said the effects wear off in about 7 days. “There was something that shocked the pupil dilator muscle,” he said. “One factor that can do this consistently is high IOP. If you had a high enough pressure, you would have corneal edema the next day or a history of complaint of pain. It would be very uncommon to have a clear cornea the next day. The vision only pinholed to 20/50, but with a clear cornea, so you have to ask why is the vision only 20/50?”
On the mydriatic front, because the first eye was a challenge to dilate, “this could have led to a more aggressive dilating regime by the nursing staff in order to achieve maximal dilation in this eye. The effects of the dilation could still be present especially if atropine or hom-atropine were used. The fact that the fellow eye has an unresponsive pupil suggests that perhaps the same sequence of events happened with that eye too following surgery and perhaps there is sphincter damage present there, too,” Dr. Cummings said.
Per Dr. Collazo, he uses a fairly typical pre-, intra-, and post-op strategy (see sidebar). The pupil reaction was rather frustrating because it was the second eye and nothing this out-of-the-ordinary was seen in the first eye, he said. “One line of thought on the etiology is that very high IOP could have caused the dilation. The worry with that is causing ischemic damage to the iris that’s permanent,” he said. Toxic anterior segment syndrome (TASS) “could also cause sphincter damage, but it sounds like the anterior segment looked okay on day 1 post-op, except for the dilated, non-reactive pupil,” Dr. Fry said, leading him to “put my money on high post-op pressure as the etiology.”
TASS is always a consideration when a patient has a persistent, dilated pupil, Dr. Mamalis said.
Dr. Cummings also suggested TASS, “or the use of hypromellose as a viscoelastic during the surgerythis has been linked to post-op dilated pupils for no other reason. Iris trauma during phaco surgery can also lead to dilated pupils but there is no mention of this.” Indeed, Dr. Collazo said aside from the (already known) issue of poor dilation, the entire surgery was uncomplicated. The patient was not a high myope, and Dr. Collazo did not perform a gonioscopy, as the patient didn’t have glaucoma. “I see many of my post-ops partially dilated on [post-op day] 1, but the pupil is usually reactive,” Dr. Collazo said. What made this case so problematic was “the pupil was more dilated than when I did the case. It looked like the patient had been on atropine for a week!”
Potential treatments
Although the natural instinct is to treat, “I would observe it initially and if there is no improvement and the post-op inflammation has subsided, I would start with pilocarpine,” Dr. Cummings said. “If this does not work and the patient is symptomatic and complaining about the enlarged pupil, then one has to consider surgical options to address this.”
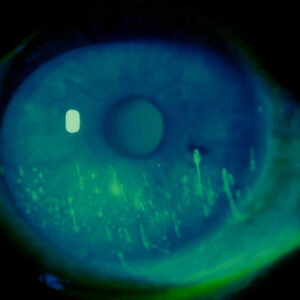
If elevated pressure caused the mydriasis, “it may never come back to normal,” Dr. Mamalis said. Dr. Fry also noted that if the dilation were a result of ischemic high pressure sphincter damage, “pilocarpine is going to be ineffective.” However, on the upside, “most cases of dilated pupils I have seen tend to do well without glare or excessive symptoms,” Dr. Fry said. He did add, however, that patients in the Midwest just don’t complain as much as in other regions of the country. “If the patients’ symptoms are excessive, I would do a pupil cerclage,” he said. Dr. Mamalis states that, cases of TASS would lead to iris damage down the road, likely with thinning and atrophy of the stroma. “In cases where chronic dilation is secondary to TASS, there will be damage to the iris itself. Surgeons may not see it on that first post-op days, but there will be subtle stromal atrophy,” he said. In his opinion what made the case unusual was a lack of corneal edema.
“I’d also recommend getting specular microscopy to look at the endothelial cell count. For someone his age, the cell count should be around 1500 or so,” he said. Treatment should depend on the patient’s symptoms, where cerclage would be recommended if the patient had serious complaints.
Outcomes
If the abnormally dilated eye was caused by a transient high post-op pressure, changing the post-op follow-up to ensure the patient is kept at the center and checked 2-3 hours after surgery before being discharged can help, Dr. Fry said. “This catches high IOP, which is fairly common, in addition to more rare problems such as retained nuclear chip, wound leak, and mal-positioned IOL,” he said. “High IOPs are treated with side port ‘burp’ and aqueous suppressants, with pressure re-check 45 minutes later before they go home.” On the rare occasion of a wound leak, the patient is “immediately” taken back into the operating room for a stitch, he said. “For the patient, an immediate return to the OR the day of surgery is viewed as a minimal re-intervention, but if they are back days later to aspirate a nuclear chip or re-position a IOL, it is viewed as more of a problem,” Dr. Fry said.
Because Dr. Collazo could not be certain a transient high IOP occurred in the immediate post-op time frame before the patient returned with the dilated pupil complication, he conducted a rigorous exam of his operating room, as though a confirmed case of TASS had been found. “One of the side effects of TASS is a persistent pupil dilation,” Dr. Mamalis said. “TASS has to be included in your differential diagnosis. You should be on the lookout for elevated pressure and corneal edema associated with it. The patient will likely have increased cell and flare as well.” During Dr. Collazo’s investigation, he discovered that the center had run out of preservative-free epinephrine and had acquired more from a different supplier. All other procedures had been “by the book” and followed recommended guidelines for autoclaving, use of preservative-free epinephrine, etc., he said.
“I had just read a review of TASS causes that was in the July issue of Journal of Cataract and Refractive Surgery, and sure enough, the review mentioned preservative-free and bisulphite-free epinephrine,” Dr. Collazo said.1 He determined the new supplier delivered preservative-free epinephrine, but not bisulphite-free.
“Although bisulphites are technically not preservatives, but are used as a stabilizing agent, it may not be at the forefront for surgeons to think about,” Dr. Mamalis said. However, the TASS Task Force recommends no products with preservatives or additives (such as bisulphites) be used in the anterior chamber. “This was a very, very mild case of TASS,” Dr. Collazo said. In this case, the pupil came down slowly, returning to almost-normal after about 6 weeks. The patient has “minimal corneal edema,” and some “diffuse mild iris atrophy,” but his current vision is 20/25.
References
- Cutler Peck CM, Brubakder J, Clouser S, Danford C, Edelhauser HE, Mamalis N. Toxic anterior segment syndrome: Common causes. J Cataract Refract Surg. 2010;36:1073-1080.
Editor’s note
The physicians interviewed have no financial interests related to their comments.
Contact information
Collazo: 787-728-3700, ecollazomd@mac.com
Cummings: +353 1 2930470, abc@wellingtoneyeclinic.com
Fry: 620-275-7248, LuFry@fryeye.com
Mamalis: 801-581-6586, nick.mamalis@hsc.utah.edu