Glaucoma: Glaucoma fundamentals
July 2016
by Stefanie Petrou Binder, MD,
EyeWorld Contributing Writer

EyeWorld is pleased to present our second “Glaucoma Fundamentals” column. The purpose of this column is to provide practical and usable tips for managing glaucoma issues in your daily practice. In this month’s column, we address the importance of recognizing and managing optic disc hemorrhages. When disc hemorrhages are seen in patients, a number of questions race through the ophthalmologist’s mind: “What exactly does this mean?” “How do I explain this to the patient without making them panic?” “What are the next diagnostic and therapeutic steps?” “Do I need to refer this patient to a specialist, and if so, how quickly?” To answer these questions, we sought the opinions of 2 world-renowned glaucoma specialists: Donald Budenz, MD, and Jody Piltz-Seymour, MD. We hope EyeWorld readers find this “Glaucoma fundamentals” helpful. We welcome your feedback and your ideas for future columns.
—Husam Ansari, MD, Glaucoma fundamentals editor
Optic disc hemorrhage is a common clinical feature of glaucoma, indicating active disease with likely progression and visual field loss. These small bleedings form notch-like lesions at the edge of the optic disc in the nerve fiber layer and often correlate with visual field loss. Their detection necessitates the utmost vigilance in patients diagnosed with glaucoma and in those who are glaucoma suspects. EyeWorld spoke with 2 glaucoma specialists to gain a better understanding of optic disc hemorrhage and its predictive value.
Disc hemorrhage and progression
“Disc hemorrhage generally indicates instability of glaucoma,” said Donald Budenz, MD, professor and chair of ophthalmology, UNC Chapel Hill, Chapel Hill, North Carolina. “Studies have shown that focal visual field defects oftentimes precede or follow the development of a disc hemorrhage at a location 180 degrees away from the disc hemorrhage on the visual field, and appear within the next 6 to 8 months. The appearance of a disc hemorrhage is therefore not pathognomonic for glaucomatous worsening, but often accompanies disease progression and should be taken as a potential sign of glaucoma instability.”
Disc hemorrhage was first described in people with normal pressure glaucoma but has been observed in high and normal pressure patients alike. According to Dr. Budenz, there is a jump in the incidence of optic disc hemorrhage in ocular hypertensives that become diagnosed with manifest glaucoma. He explained, “Our work in the Ocular Hypertension Treatment Study showed that the yearly incidence of new optic disc hemorrhages in ocular hypertensives was 0.5%. Once a patient developed manifest primary open angle glaucoma, it rose to 2.5% per year.”1
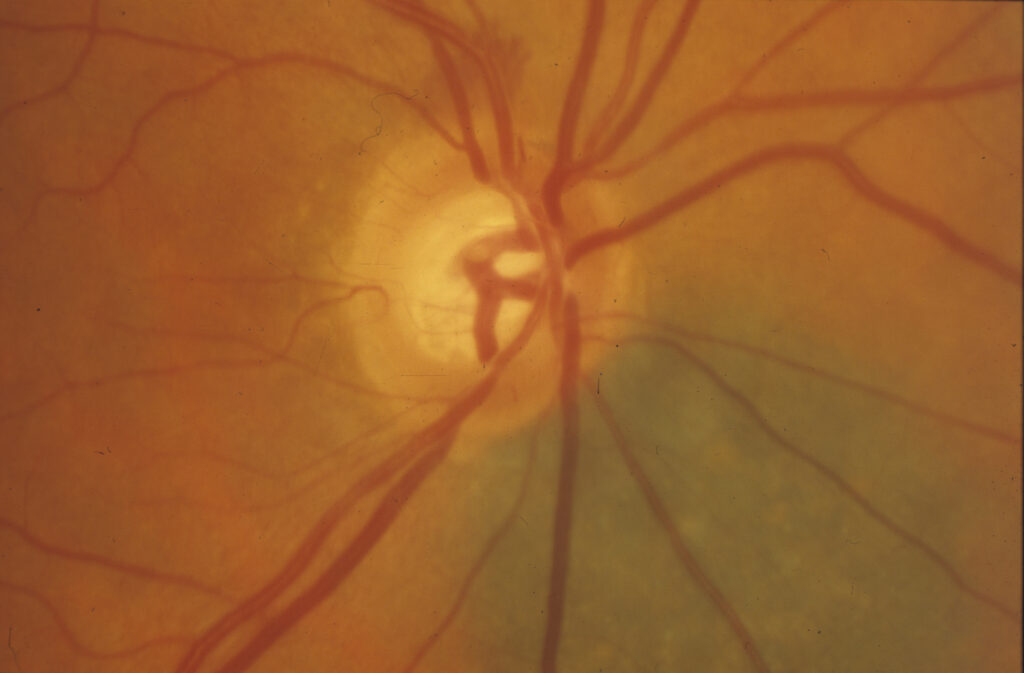
Source: Donald Budenz, MD
Patient management
Disc hemorrhages resolve by themselves and require no treatment, Dr. Budenz said. However, once spotted, the physician should consider keeping a more careful watch over the patient and fine-tuning the treatment regimen. “In the setting of a glaucoma suspect, one would monitor that patient more closely, and if the patient had other risk factors that put him or her at high risk for development of glaucoma, one could consider instituting treatment,” Dr. Budenz said.
He added, “In a patient with manifest glaucoma, either the pressure is not adequately controlled for much of the time during the day or the pressures are fluctuating and causing instability in the glaucoma. Physicians might want to escalate therapy in that case by adding a medication to the existent regimen or performing laser surgery trabeculoplasty.”
The challenge is trying to get the pressure stable throughout the day. He said, “Even if the pressure seems adequately controlled in the office, one generally has to assume that the pressure is not as well-controlled 24 hours a day, particularly when patients are supine or while sleeping, which can cause pressures to rise.”
Once he has identified an optic disc hemorrhage for which treatment is indicated, Dr. Budenz escalates the treatment and sees patients roughly 1 month later to assess if the IOP is responding. He explained that in chronic glaucoma management, scrutinizing the optic nerve is a priority. “Because of new information about how disc hemorrhages are associated with damage, many physicians these days will take a look at the fundus even through the undilated pupil, just to look for hemorrhages and to confirm that this ‘sign’ is not present.”
Spotting a disc hemorrhage
Spotting an optic disc hemorrhage takes a careful eye, according to Jody Piltz-Seymour, MD, Valley Eye Professionals, Huntingdon Valley, Pennsylvania, and Wills Eye Hospital Glaucoma Service, Philadelphia. She said that finding disc hemorrhages requires extra special attention. “Disc hemorrhages are usually missed if you just look at the disc casually. They can be subtle and mimic blood vessels. When I teach residents, I tell them to look at the disc as part of the regular assessment, and then stop and scrutinize the disc specifically for disc hemorrhages. If you don’t take that step, you are going to miss them. Certainly, the best way to find them is by taking optic disc photographs and studying them under high magnification. In fact, in the Ocular Hypertension Treatment Study, the vast majority of photographically documented disc hemorrhages were missed on examination. Only 17% of those identified on photographs were spotted on examination.”
She explained that disc hemorrhages were relatively common, and their full incidence was hard to nail down because of their transient nature, coming and going within a matter of weeks. Their incidence seems to be higher in women, increased with age, and more prominent in people with vascular spastic issues like migraine headache. Females with regular migraines tend to have glaucoma at lower pressures, and they are more prone to disc hemorrhages, she said.
Disc hemorrhages form nerve fiber layer defects, according to Dr. Piltz-Seymour. “At the spot where you see a disc hemorrhage, there may be no change at first. Later on, though, you may find a notch or an extension of a notch where the disc hemorrhage was. Disc hemorrhages don’t form in notches, they form at the edge of notches—you have to have rim tissue for the disc hemorrhage to form. You’ll see that if the disc hemorrhage was at the edge of a notch, the notch is now wider—the nerve fiber layer defect is wider. There may also be some increase in beta peripapillary atrophy.”
Telling the patient
Disc hemorrhages are very predictive of future progression in patients with glaucoma, causing visual field worsening, increased cupping, decreased nerve fiber layer, increased beta peripapillary atrophy, and an increased risk of changing from glaucoma suspect to manifest glaucoma. Patients therefore need to be informed about the relevance of disc hemorrhage, but without unnecessarily alarming them.
Informing patients is a balancing act that Dr. Piltz-Seymour thinks is best done with tact. “The minute you use the word ‘hemorrhage,’ patients think of something big and massive. So I explain that there is a small marker, a little droplet of blood on their optic disc, which although tiny is a warning flag that everything may not be rock stable. I explain the need to follow them a bit more closely and maybe be a little bit more aggressive, if we can be.”
Reference
1. Budenz DL, et al. Detection and prognostic significance of optic disc hemorrhages during the Ocular Hypertension Treatment Study. Ophthalmology. 2006;113:21372143.
Editors’ note
Drs. Budenz and Piltz-Seymour have no financial interests related to their comments.
Contact information
Budenz: 919-966-5296
Piltz-Seymour: Jody.Piltz@outlook.com



